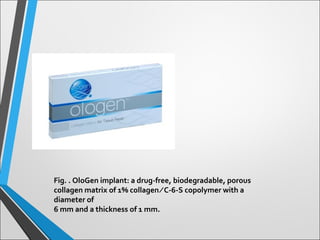
1) Trabeculectomy is the most common glaucoma surgery but scarring can lead to bleb failure. OloGen collagen implant may help control wound healing to maintain drainage.
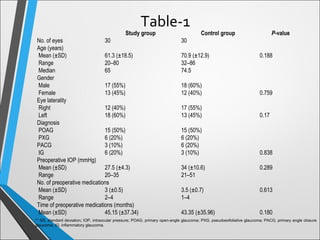
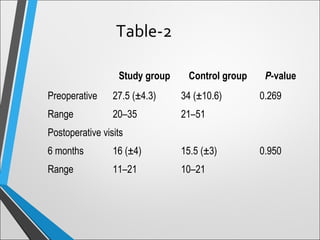
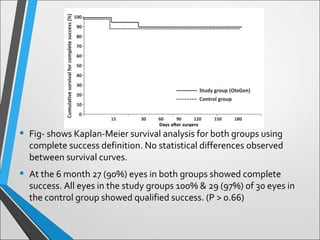
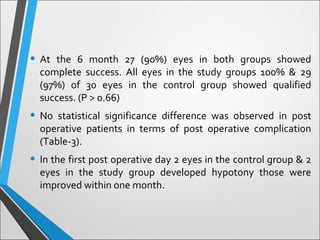
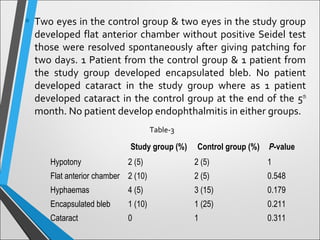
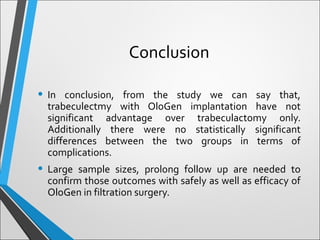
2) This study compares outcomes of trabeculectomy with and without OloGen implant in 60 eyes over 6 months. Success rates and complications were similar between groups with no significant differences.
3) While OloGen did not provide clear advantages in this pilot study, larger trials with longer follow up are needed to fully evaluate its safety and efficacy in trabeculectomy.