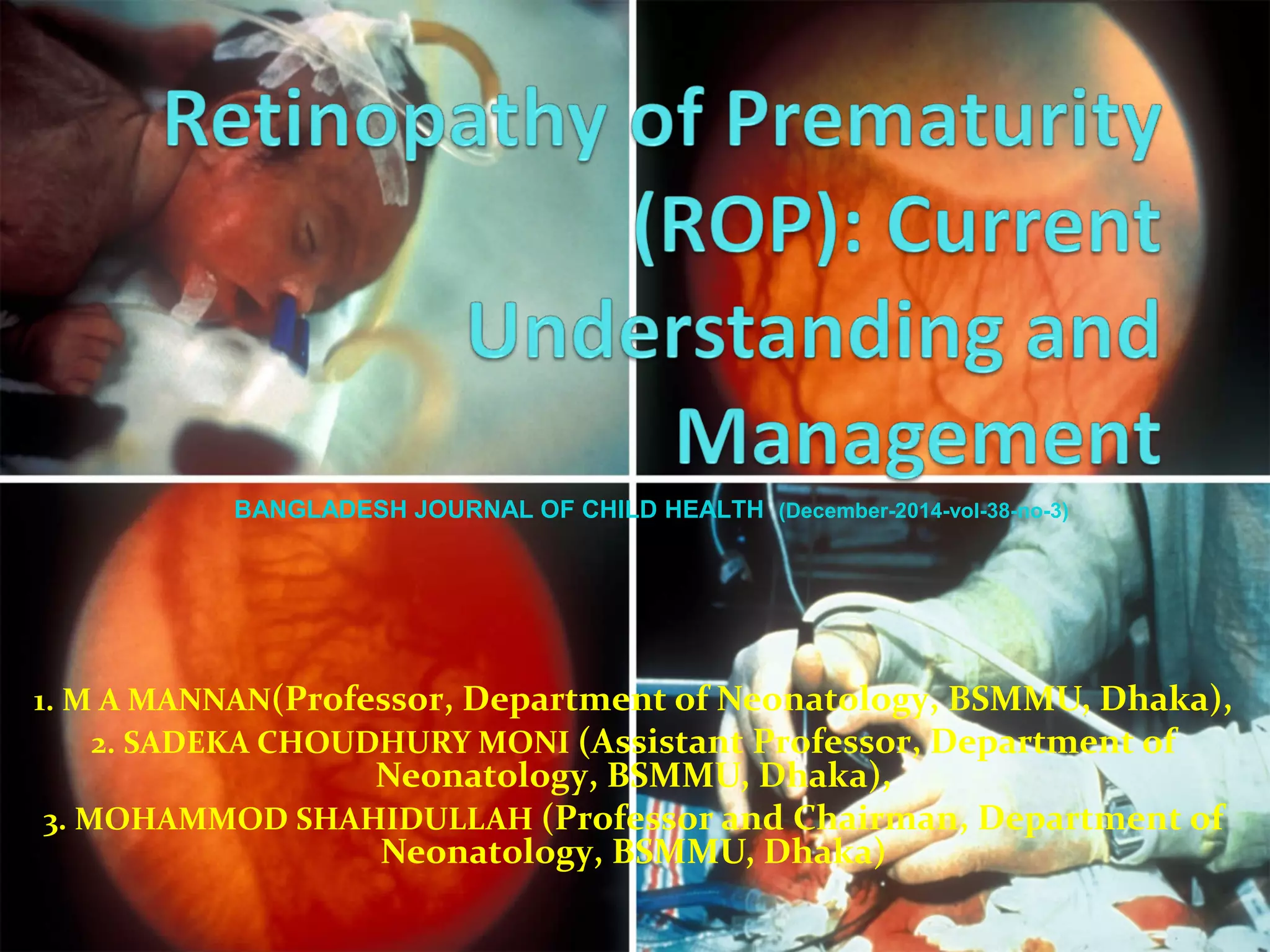
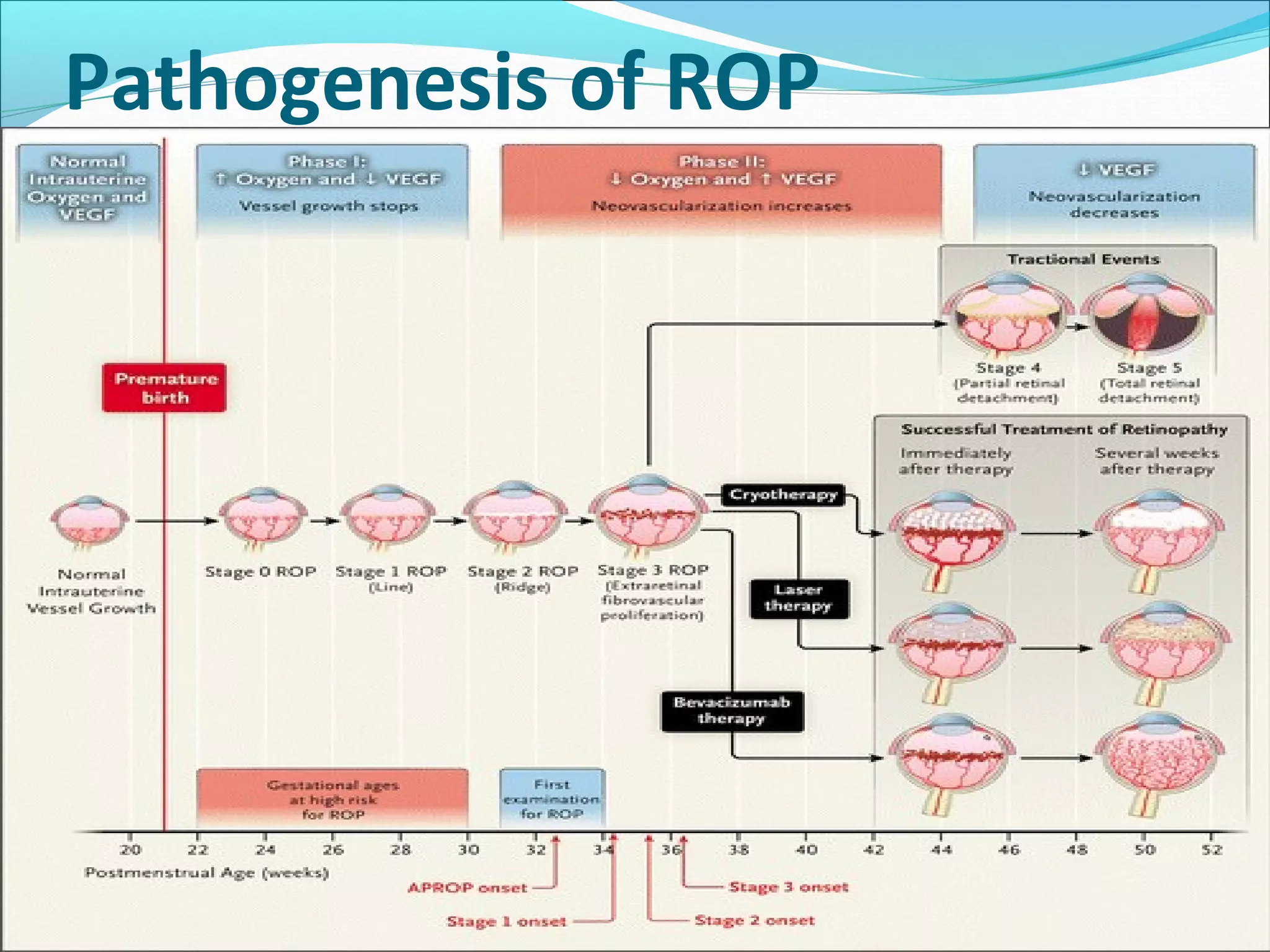
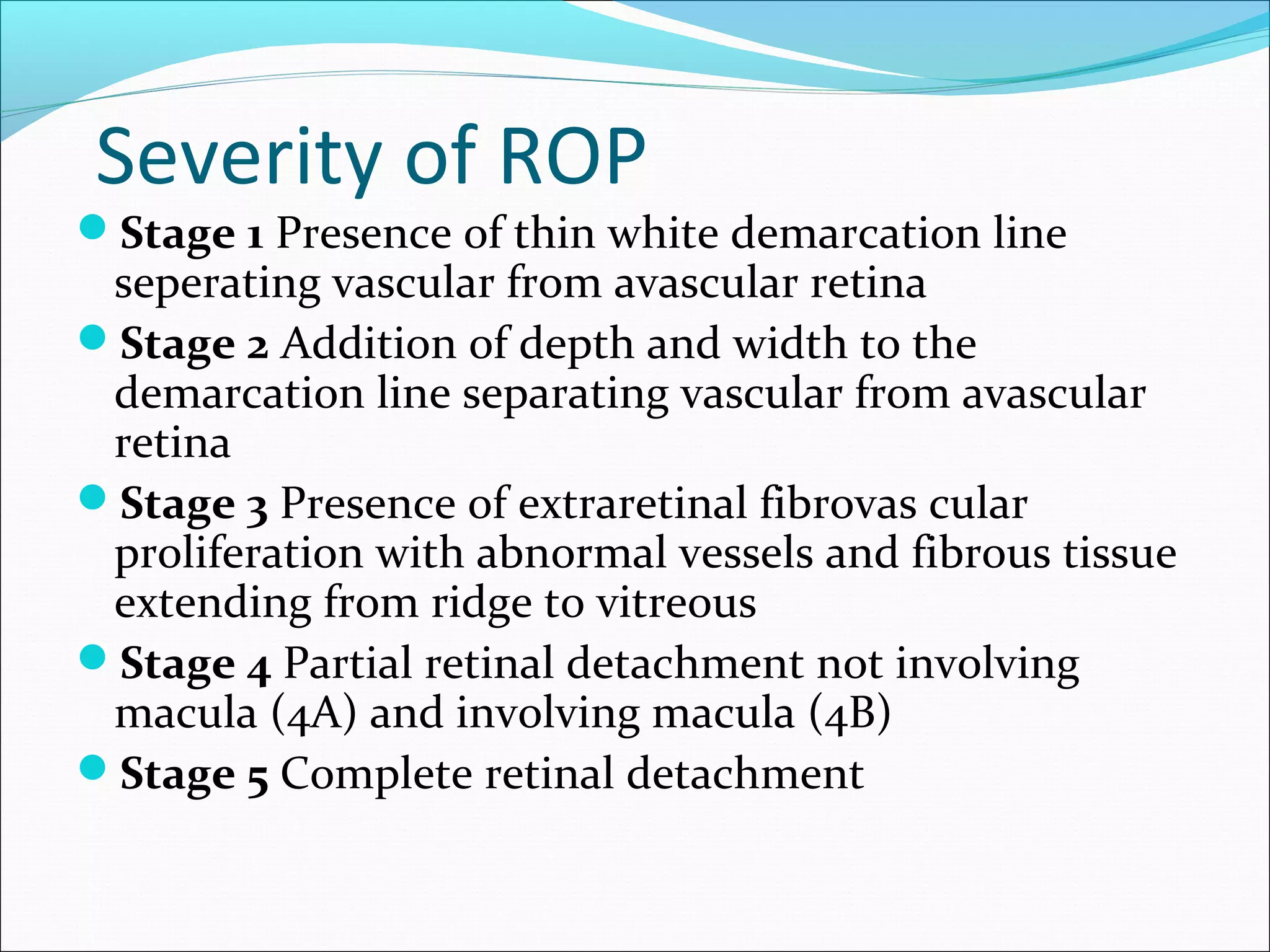
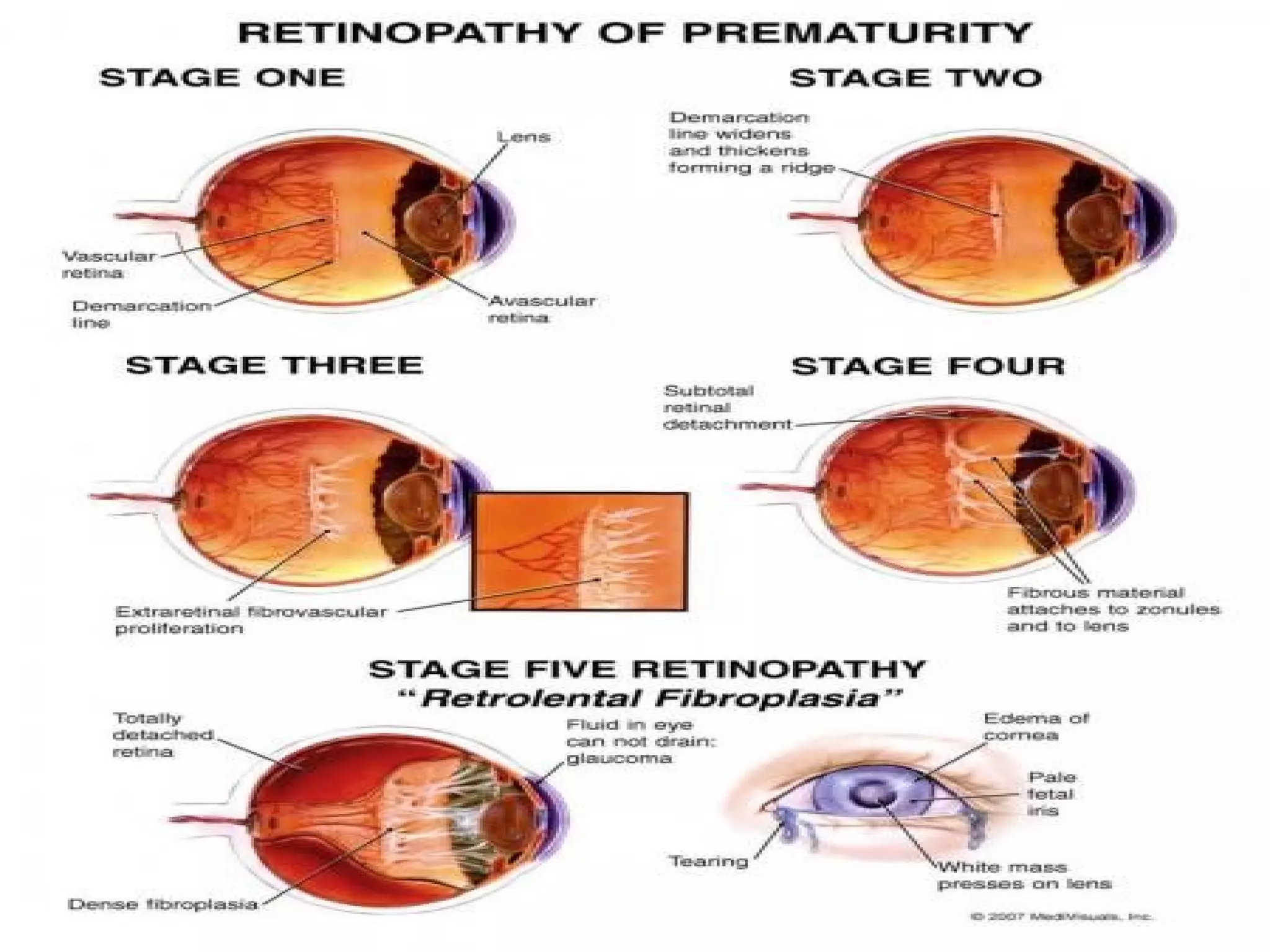
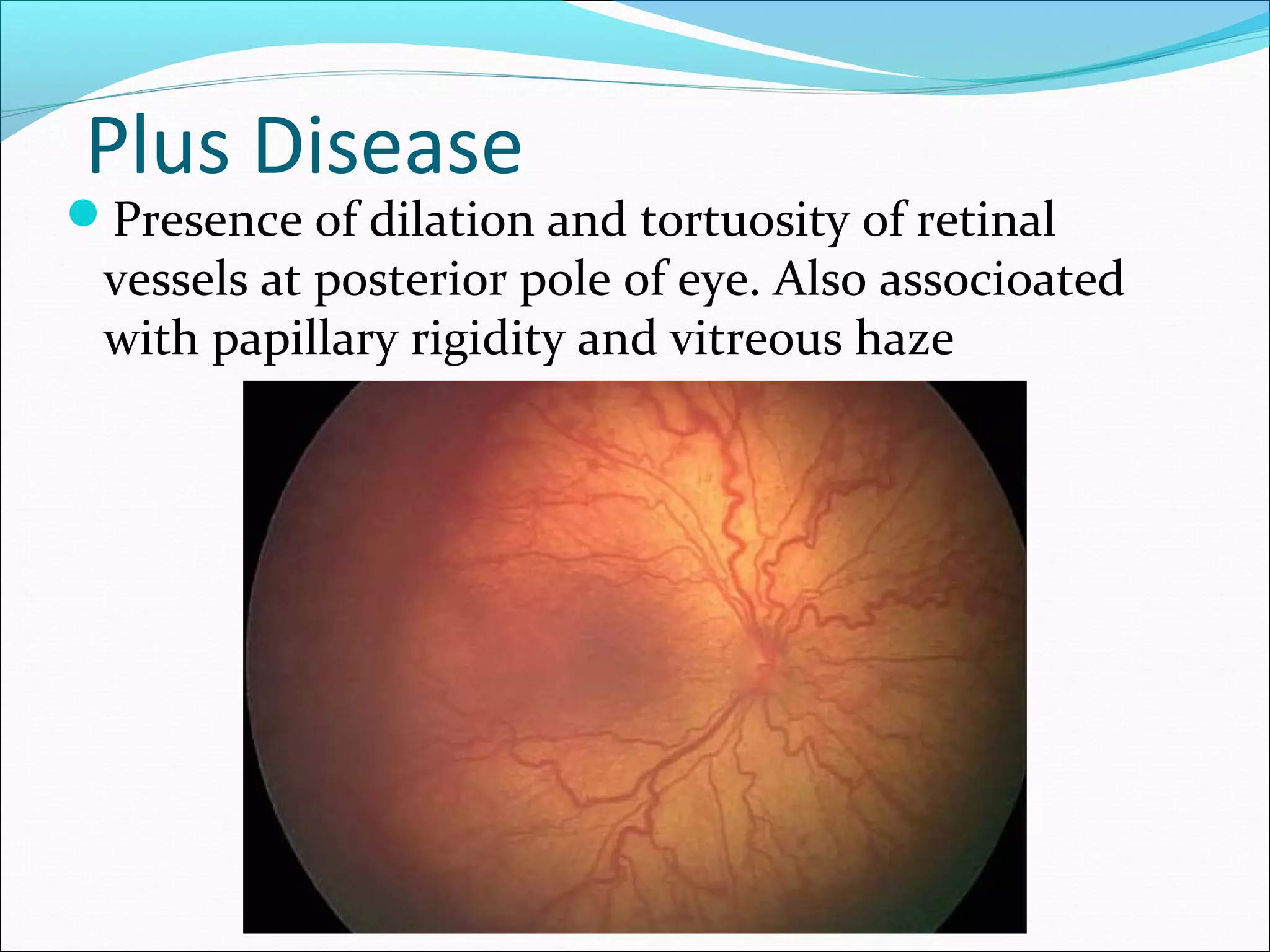
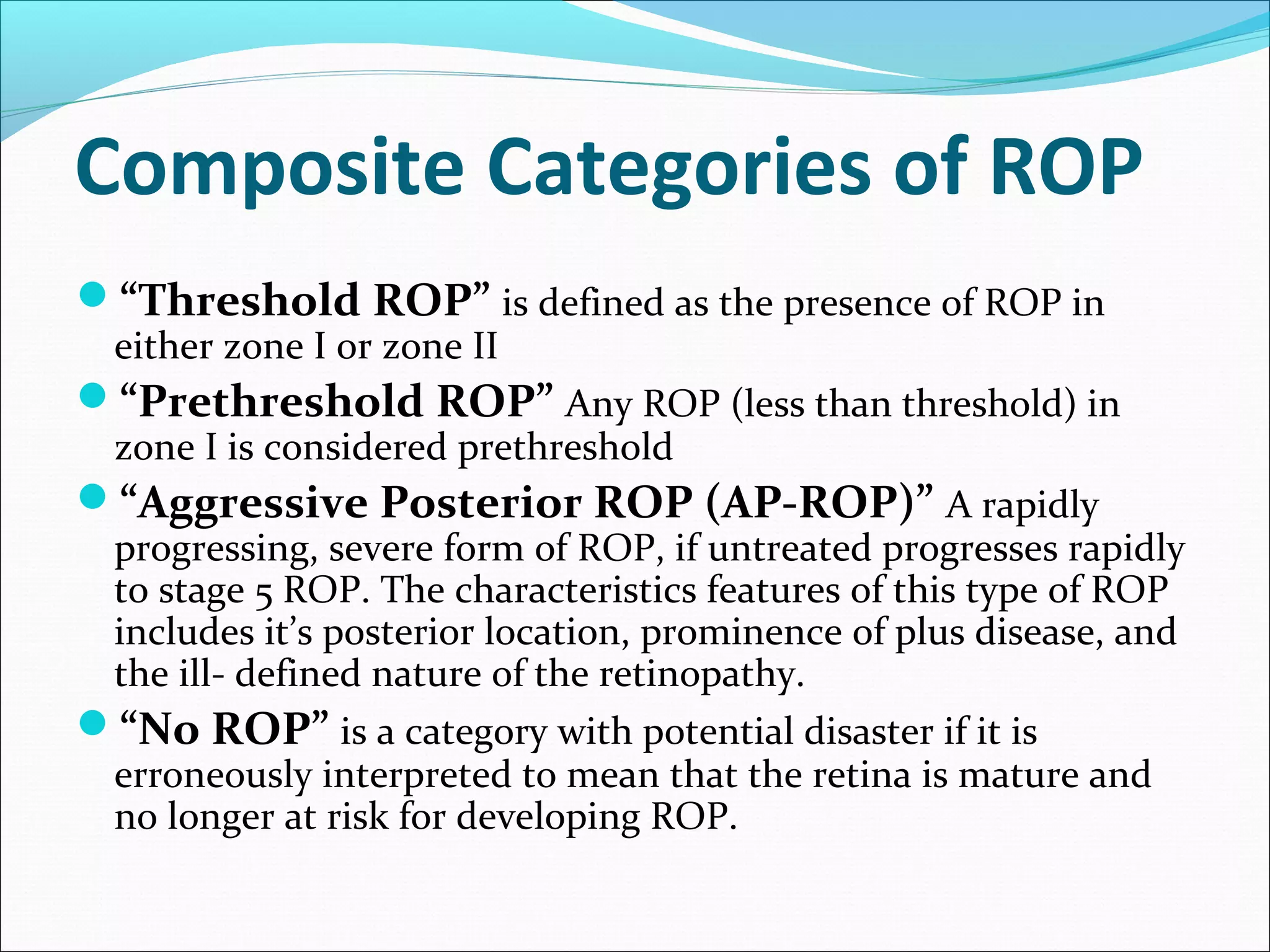
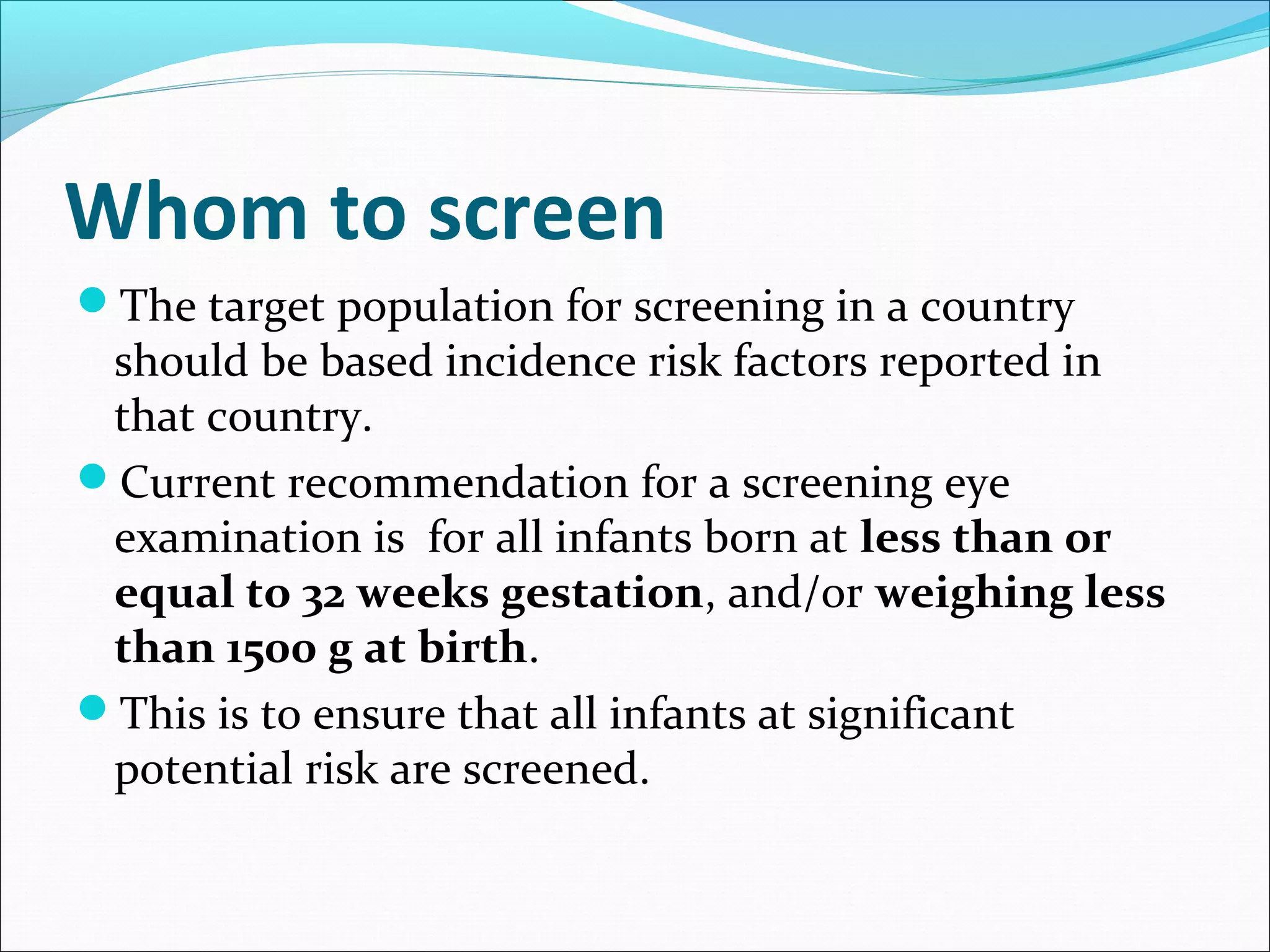
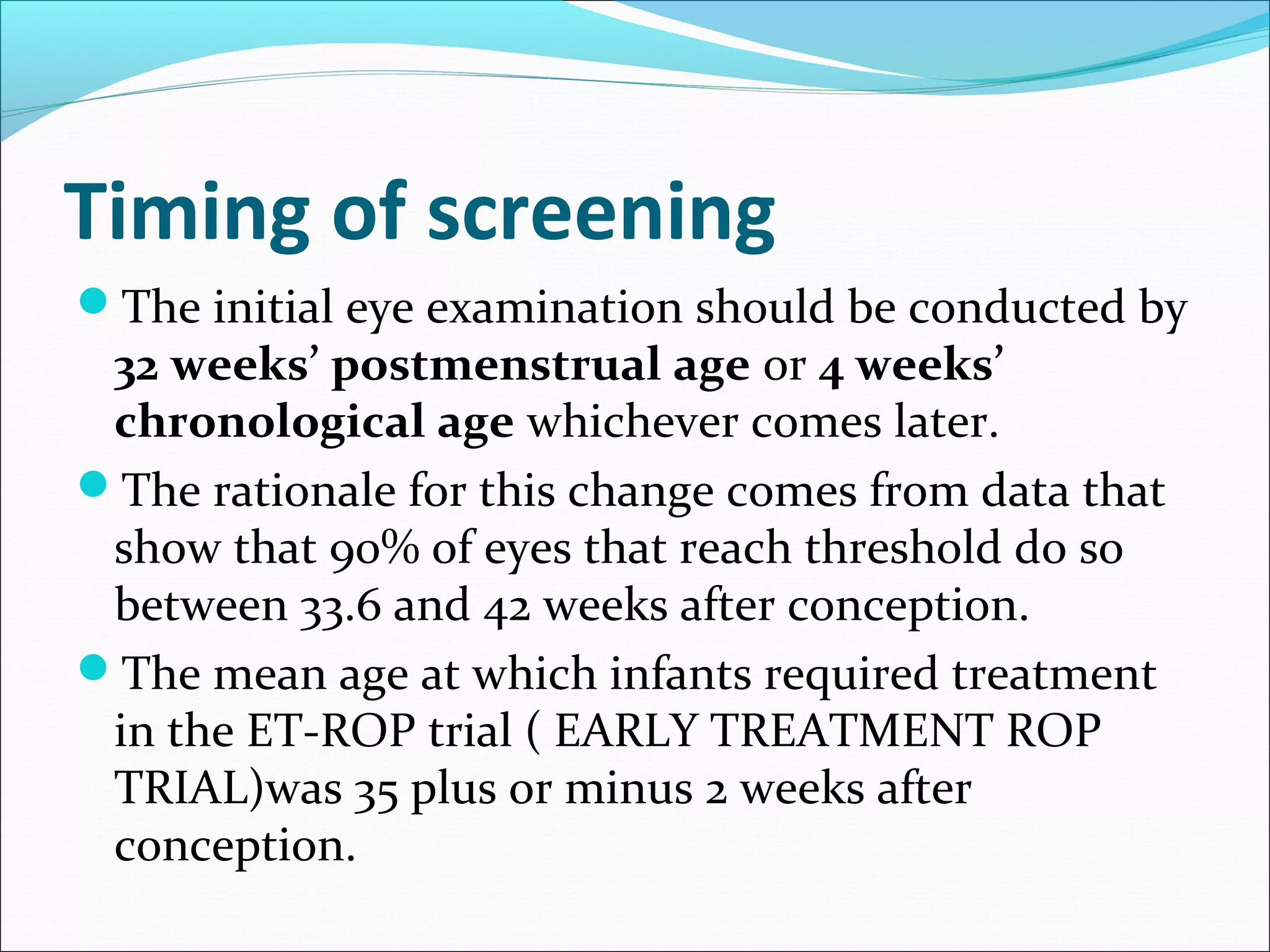
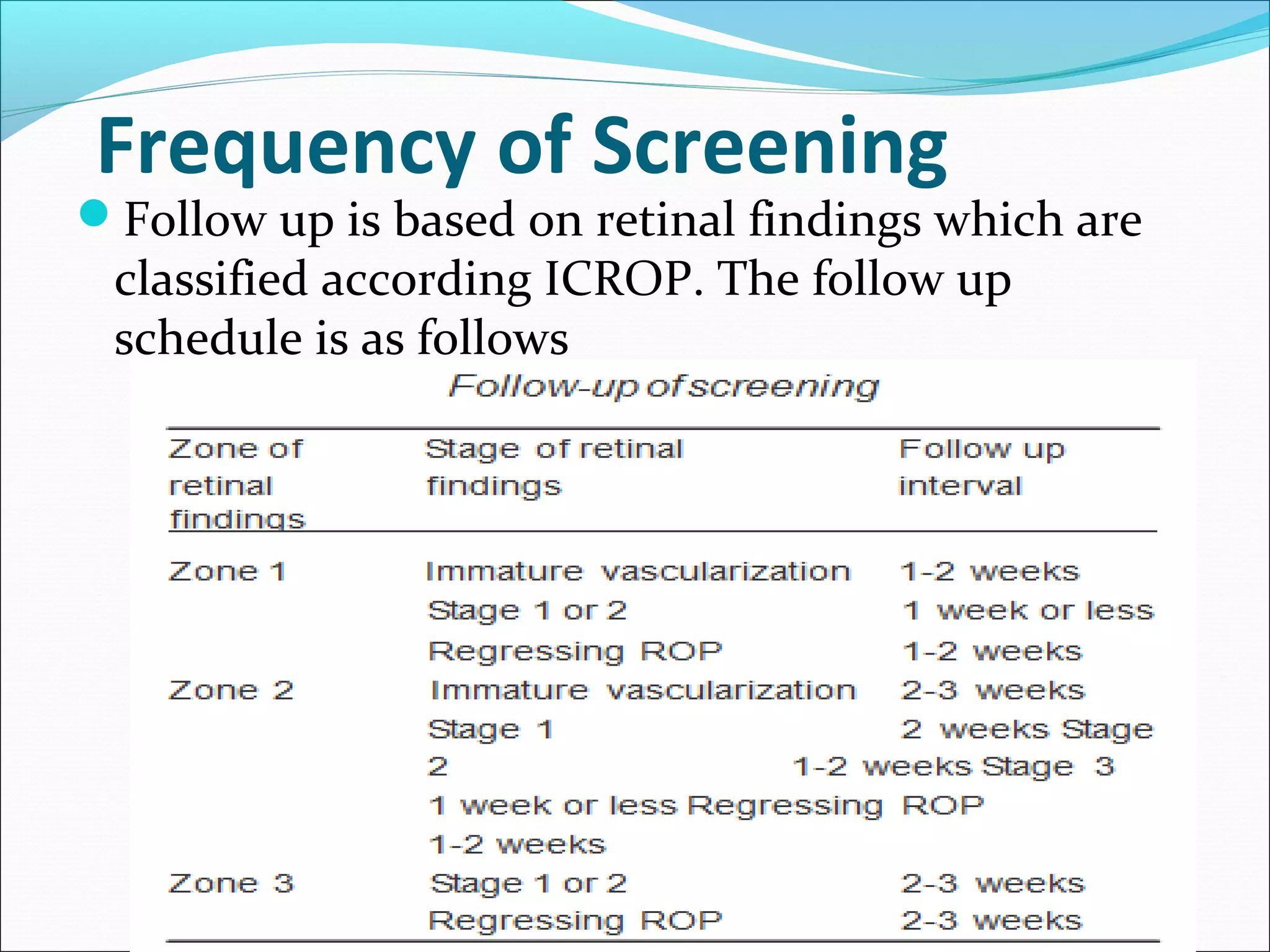
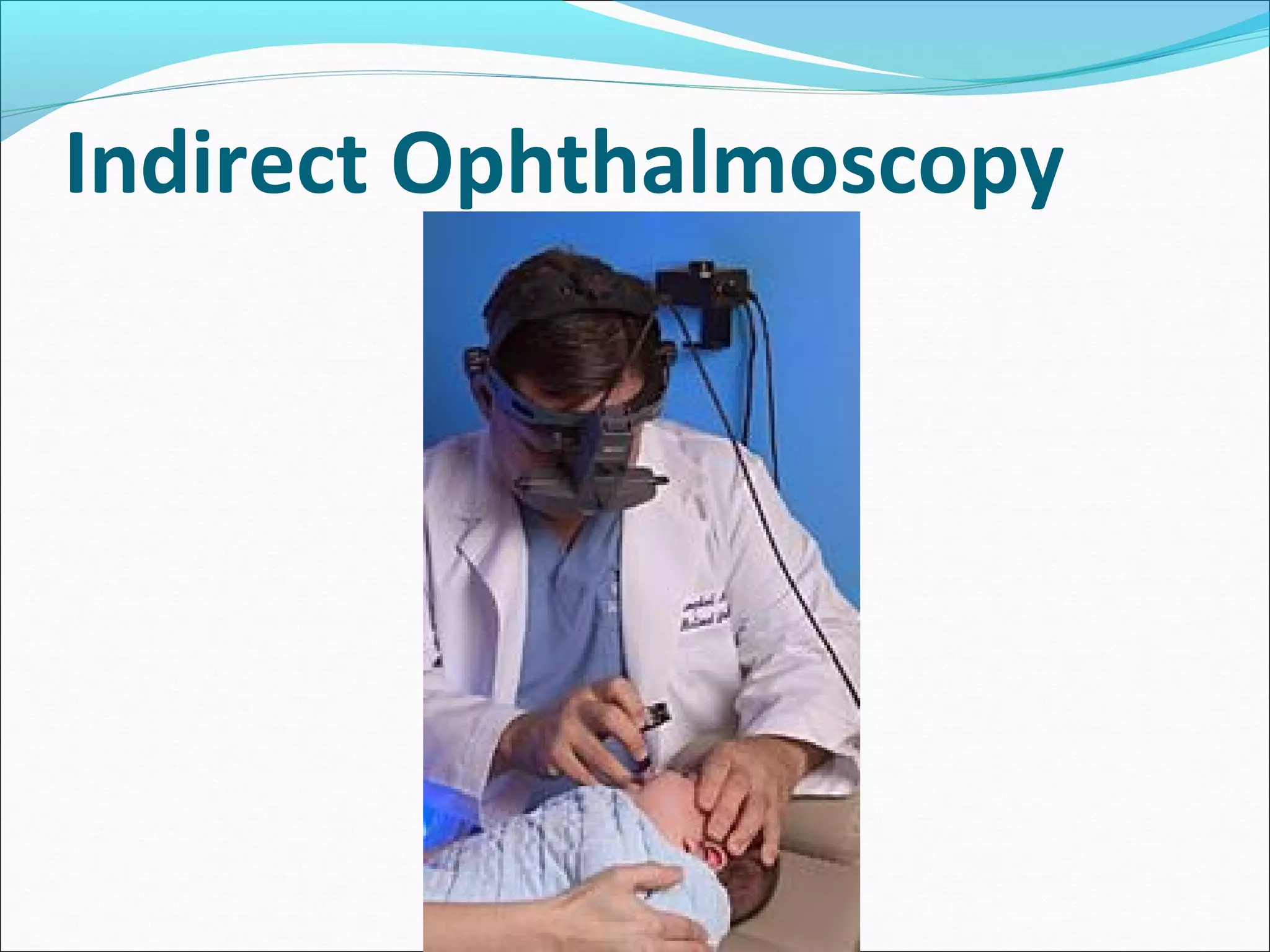
Retinopathy of prematurity (ROP) is a serious vascular eye disease affecting preterm infants, leading to blindness and severe visual impairment due to abnormal retinal blood vessel development. The document details the epidemiology, risk factors, screening, and treatment of ROP, emphasizing the need for early detection and intervention to prevent disability. It highlights the challenges in managing ROP, especially in developing countries like Bangladesh, where increased survival rates of preterm infants have led to a rising incidence of the disease.