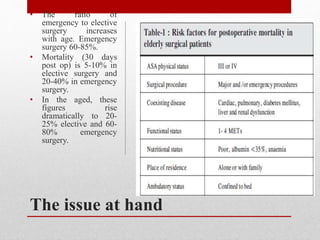
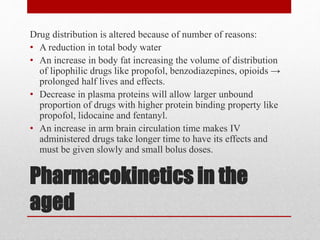
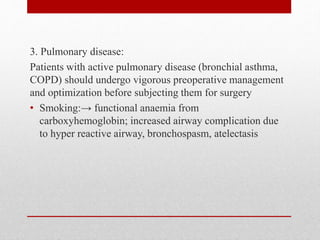
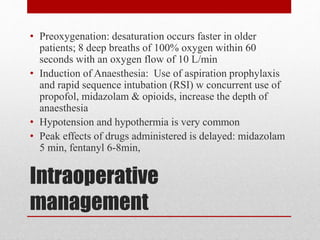
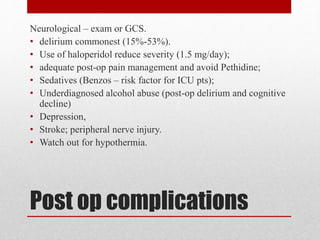
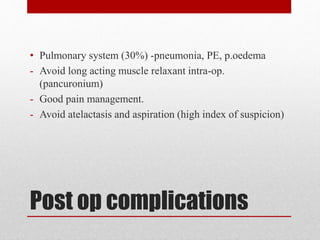
Geriatric anaesthesia requires special consideration due to age-related physiological changes that increase risks for elderly patients undergoing surgery. Pre-operative assessment is important to identify risk factors like cardiovascular, pulmonary, renal and neurological conditions. During surgery, risks of hypotension, hypothermia and delayed drug effects must be managed. Post-operatively, risks include delirium, pneumonia, cardiac complications, and other issues that require close monitoring. Regional anesthesia may provide some benefits over general anesthesia for elderly patients by reducing certain risks. Thorough pre-operative evaluation and optimization of patient conditions can help improve outcomes for elderly surgical patients.

![Reference
1. Wilkinson K, Martin I, Gough M, et al. An age old problem: A review of the
care received by elderly patients undergoing surgery. London: NCE-POD;
2010. [Accessed August 13, 2015]. Available from:1.
http://www.ncepod.org.uk/2010report3/downloads/EESE_fullReport.pdf.
[Google Scholar]
2. Kumra, V.P., (2008) issues in geriatric anaesthesia. KSAUAMRRCA J .:
AISnSaUesEtSh . I2N0 0G8E; R1I (A1T) R: 3IC9 -A 4N9AESTHESIA
3. Sieber F.E., Barnett S.R. (2012). Preventing postoperative complications in the
elderly . NCBI. Available from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3073675/
4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4806808/
5. https://www.slideshare.net/mubarakkerim/surgery-in-the-
elderly?from_action=save](https://image.slidesharecdn.com/geriatricanesthesiawithspecialconsideration-200828002657/85/Geriatric-anesthesia-with-special-consideration-Petrus-Iitula-28-320.jpg)