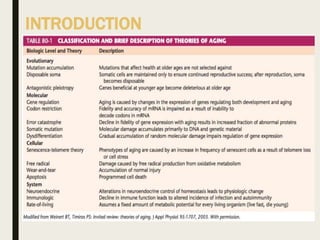
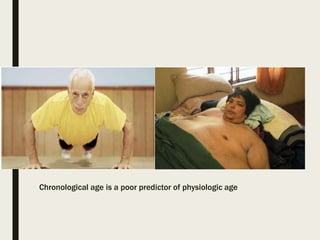
The document discusses geriatric anesthesia and the anatomical and physiological changes that occur with aging. Key points:
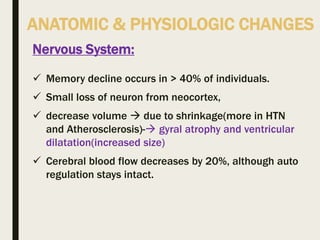
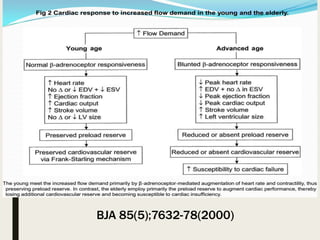
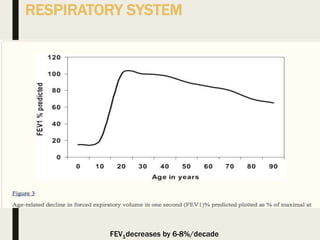
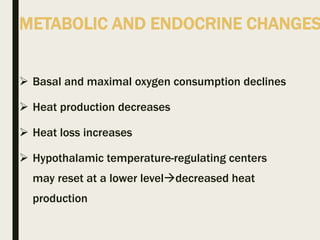
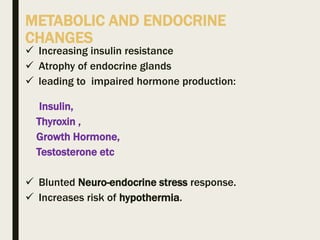
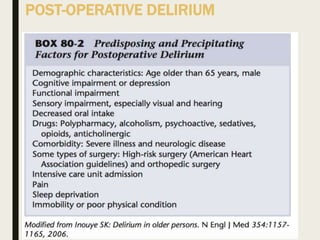
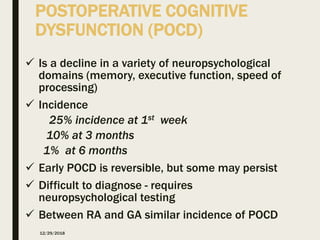
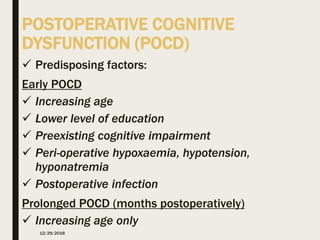
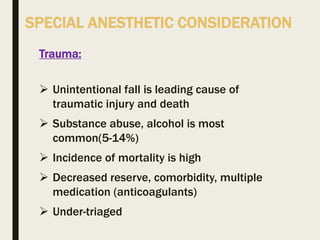
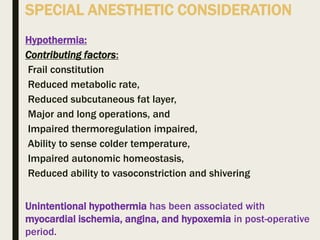
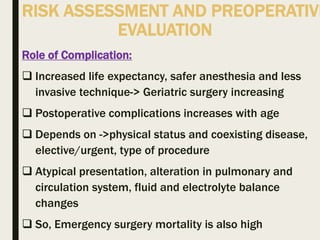
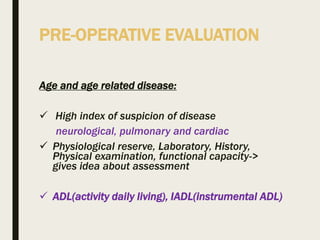
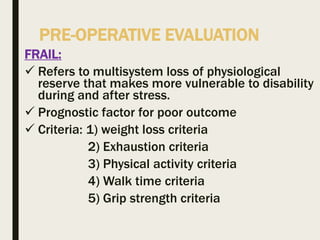
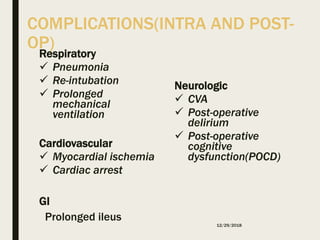
- Aging is associated with a progressive decline in organ system function and physiological reserves. This limited reserve is most evident during times of physiological stress like surgery.
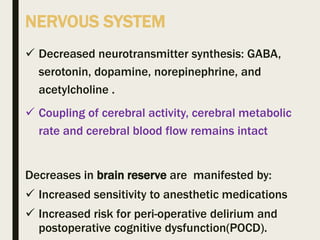
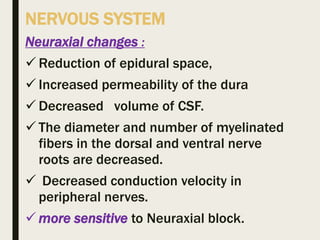
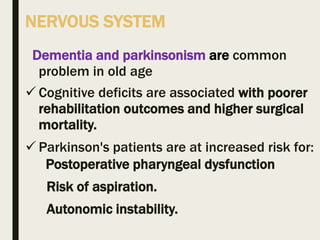
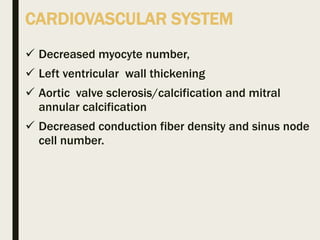
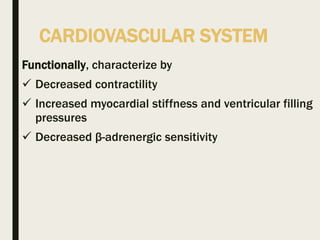
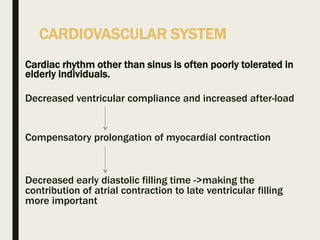
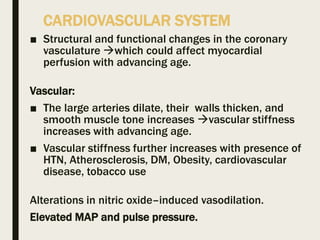
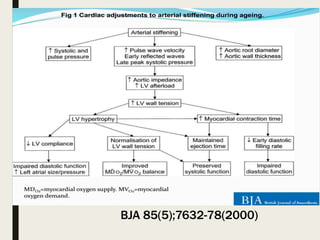
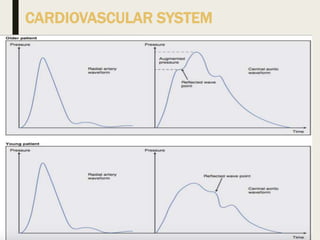
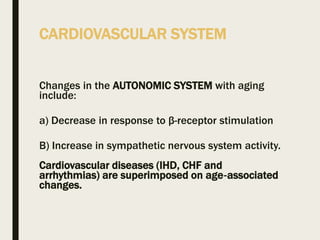
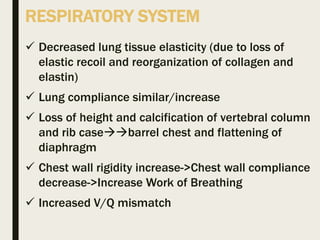
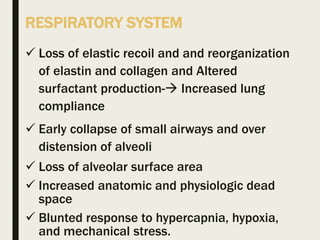
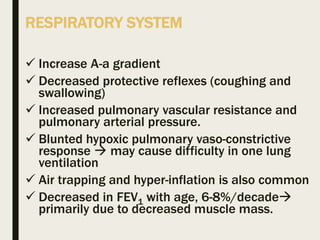
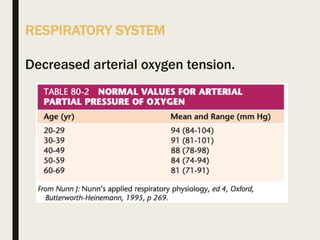
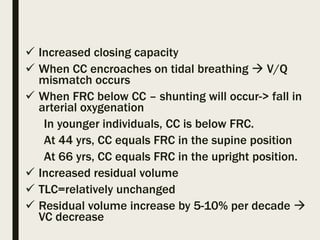
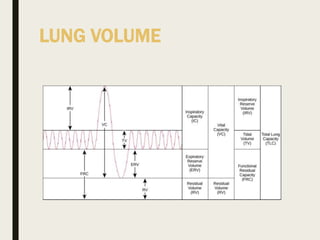
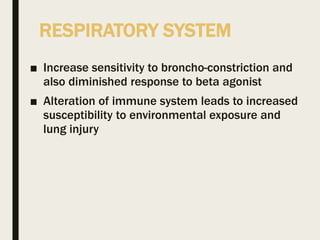
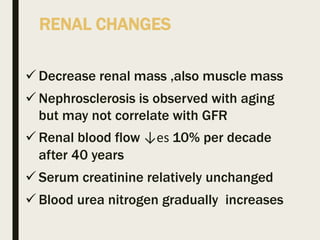
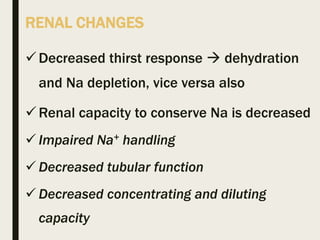
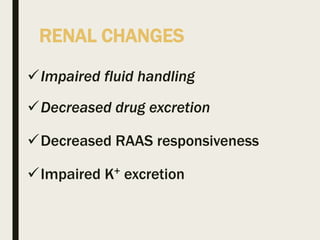
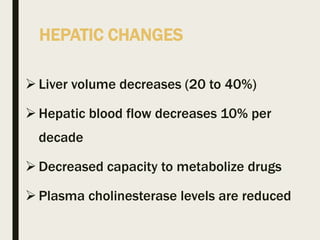
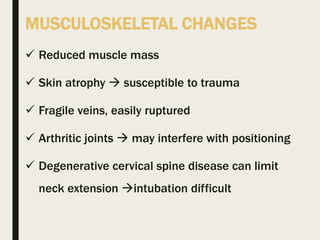
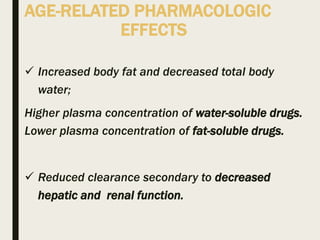
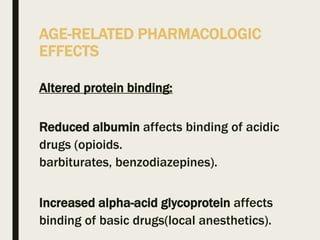
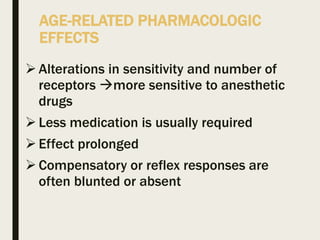
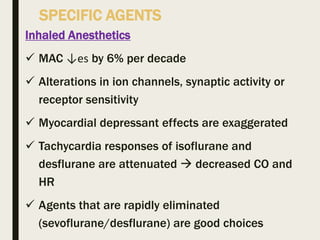
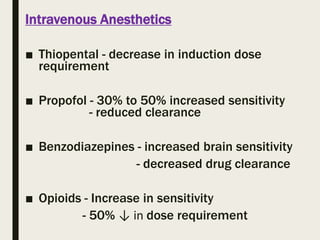
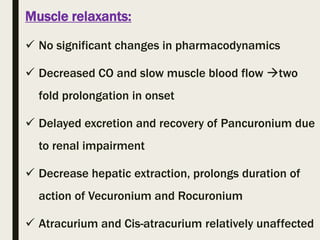
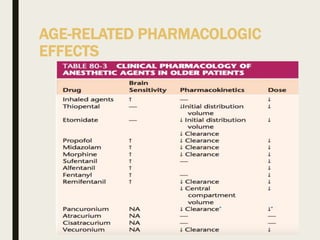
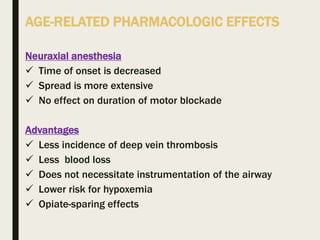
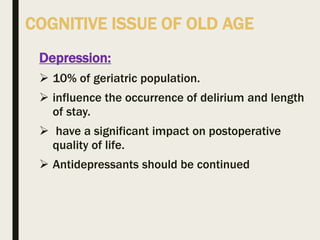
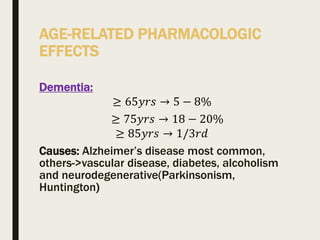
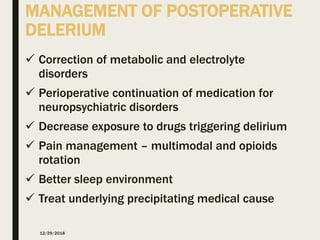
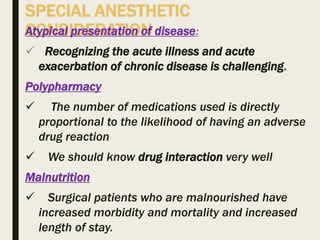
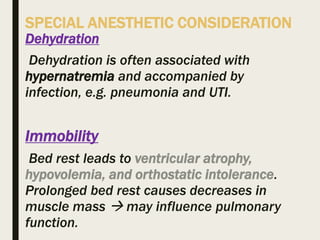
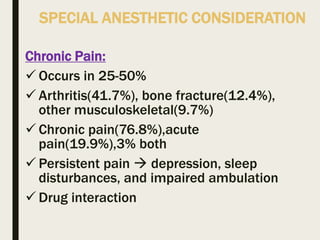
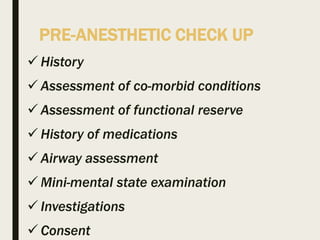
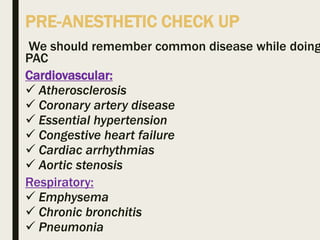
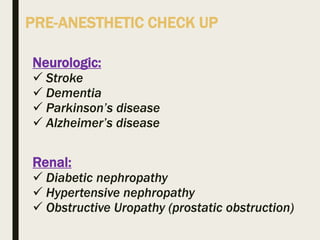
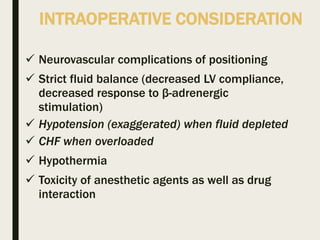
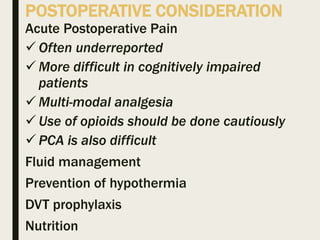
- Common changes include decreased brain, liver and kidney function, increased sensitivity to medications, and altered cardiovascular, respiratory and endocrine systems.
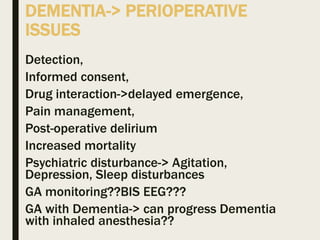
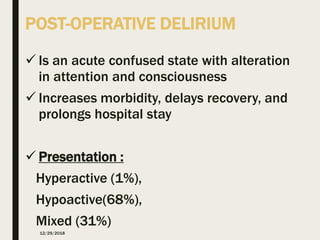
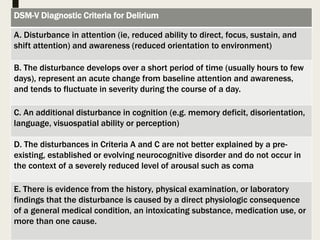
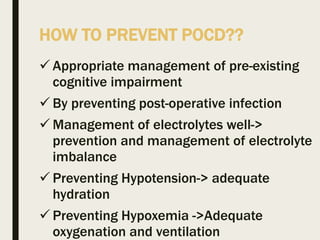
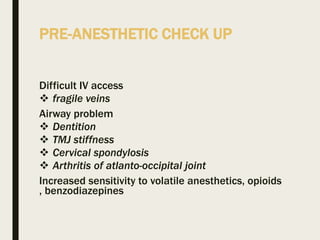
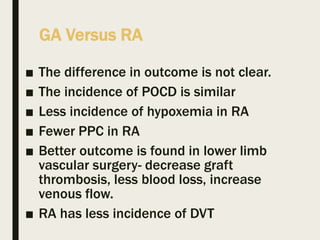
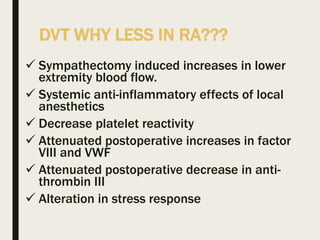
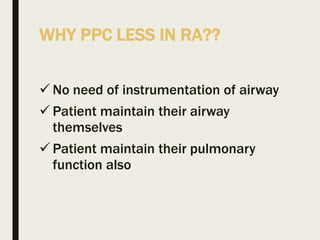
- These anatomical and physiological alterations are important considerations for preoperative evaluation, intraoperative management, and postoperative care of elderly patients undergoing anesthesia and surgery. Close monitoring and adjusted dosing of medications are often needed.