This document provides an overview of geriatric anaesthesia. It discusses the physiological changes that occur with aging and their implications for anaesthesia management. Key points include:
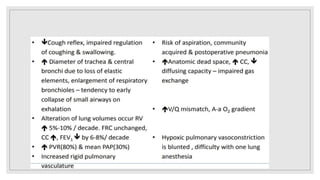
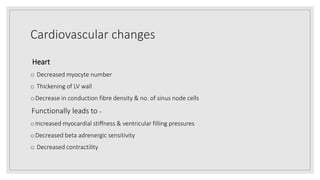
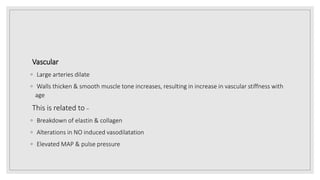
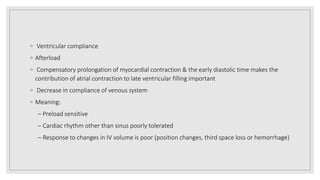
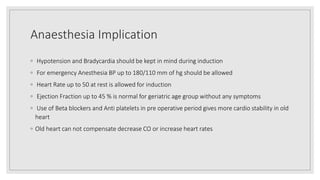
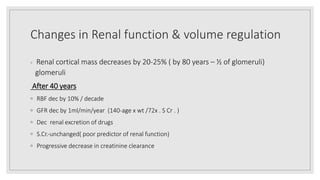
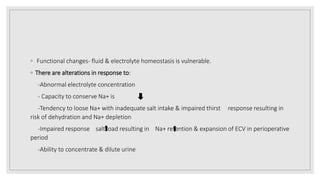
1. Organ systems like the cardiovascular, respiratory and renal systems undergo age-related changes that reduce functional reserve and increase vulnerability to haemodynamic fluctuations.
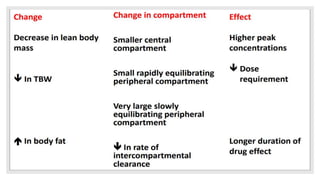
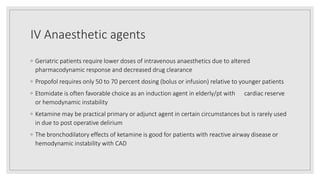
2. Anaesthetic pharmacokinetics and pharmacodynamics are also altered in elderly patients, requiring lower doses of drugs.
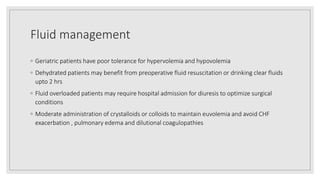
3. Thorough preoperative assessment of medical history, functional status and frailty is important for risk stratification and care planning. Close perioperative monitoring and attention to fluid balance, temperature regulation and delirium prevention are also crucial.