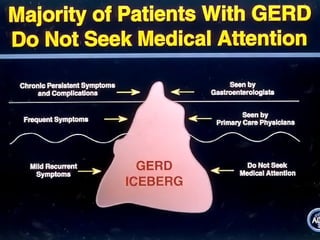
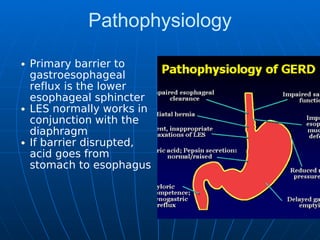
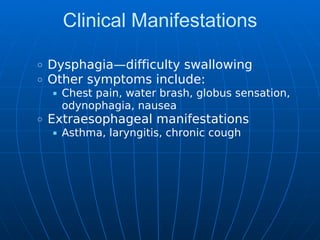
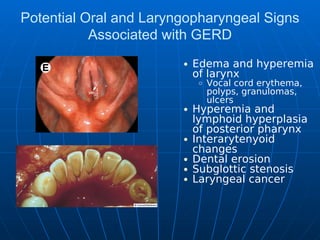
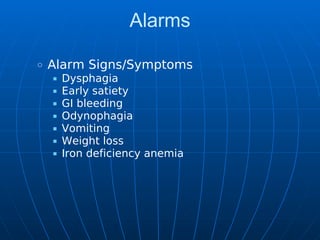
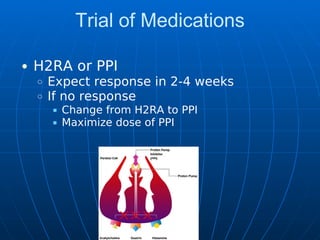
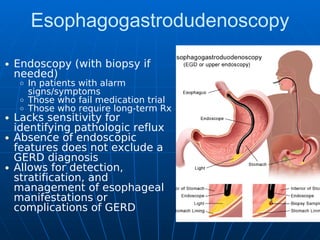
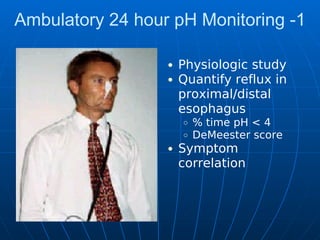
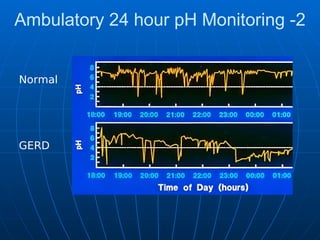
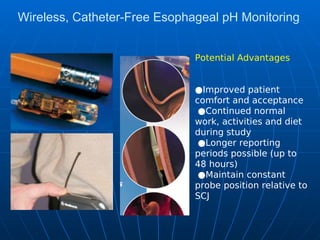
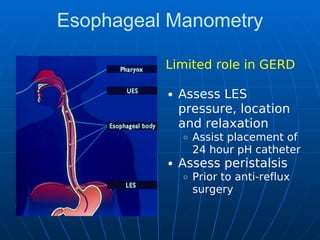
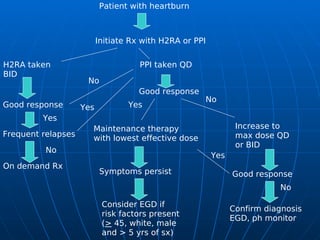
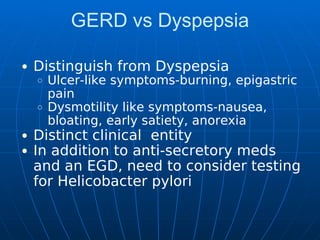
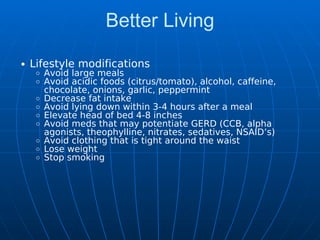
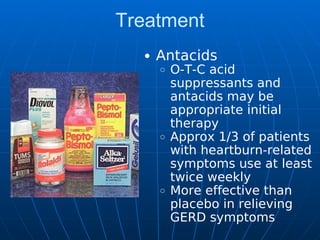
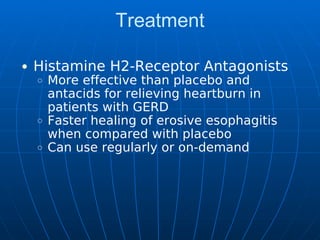
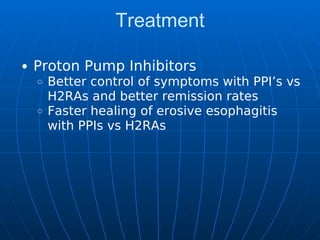
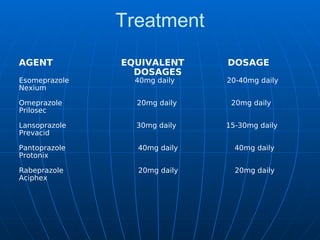
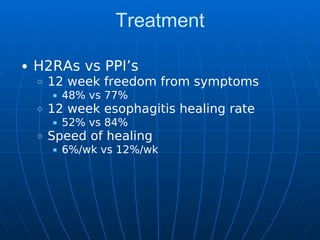
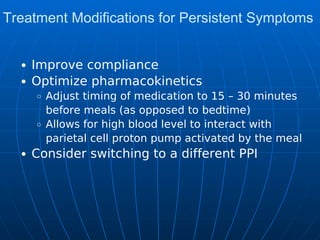
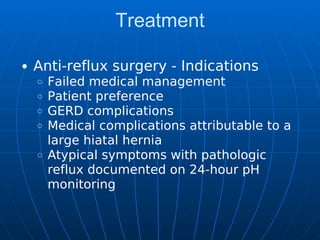
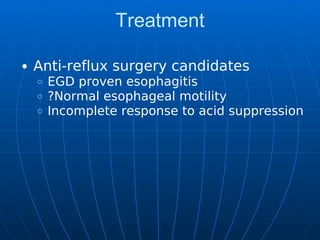
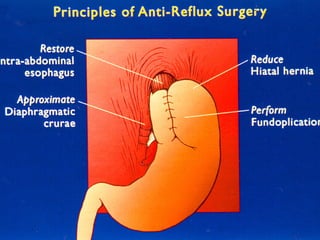
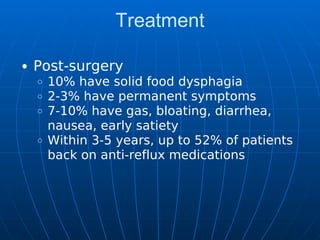
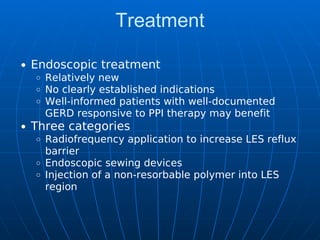
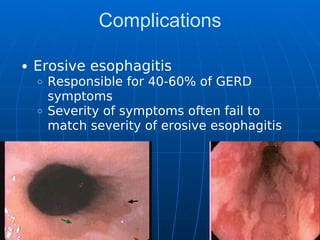
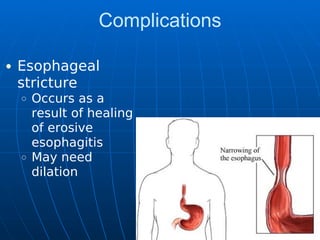
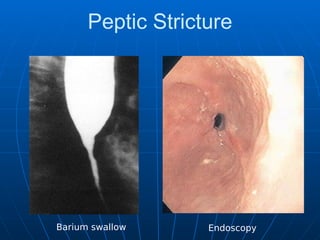
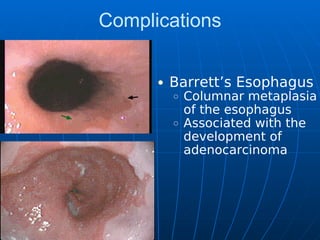
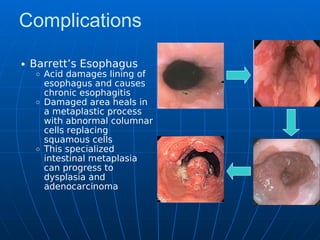
Gastroesophageal reflux disease (GERD) is characterized by the abnormal reflux of gastric contents into the esophagus, leading to symptoms like heartburn and regurgitation. The document outlines the epidemiology, clinical manifestations, diagnostic evaluations, treatment options including medications and lifestyle modifications, as well as complications associated with GERD. It emphasizes the importance of differentiating GERD from other conditions, such as dyspepsia, and the role of surgeries for cases resistant to medication.