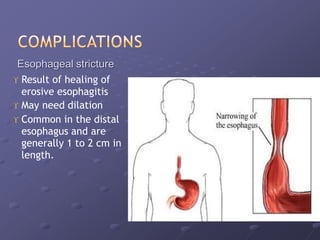
This document discusses atypical presentations of gastroesophageal reflux disease (GERD). It defines GERD and notes that while heartburn is the classic symptom, GERD can present with other symptoms or complications in patients who lack typical symptoms. It describes how GERD can manifest as cough, asthma, laryngitis, dental erosion or non-cardiac chest pain and outlines the diagnostic tests and treatment approaches for both typical and atypical GERD presentations.