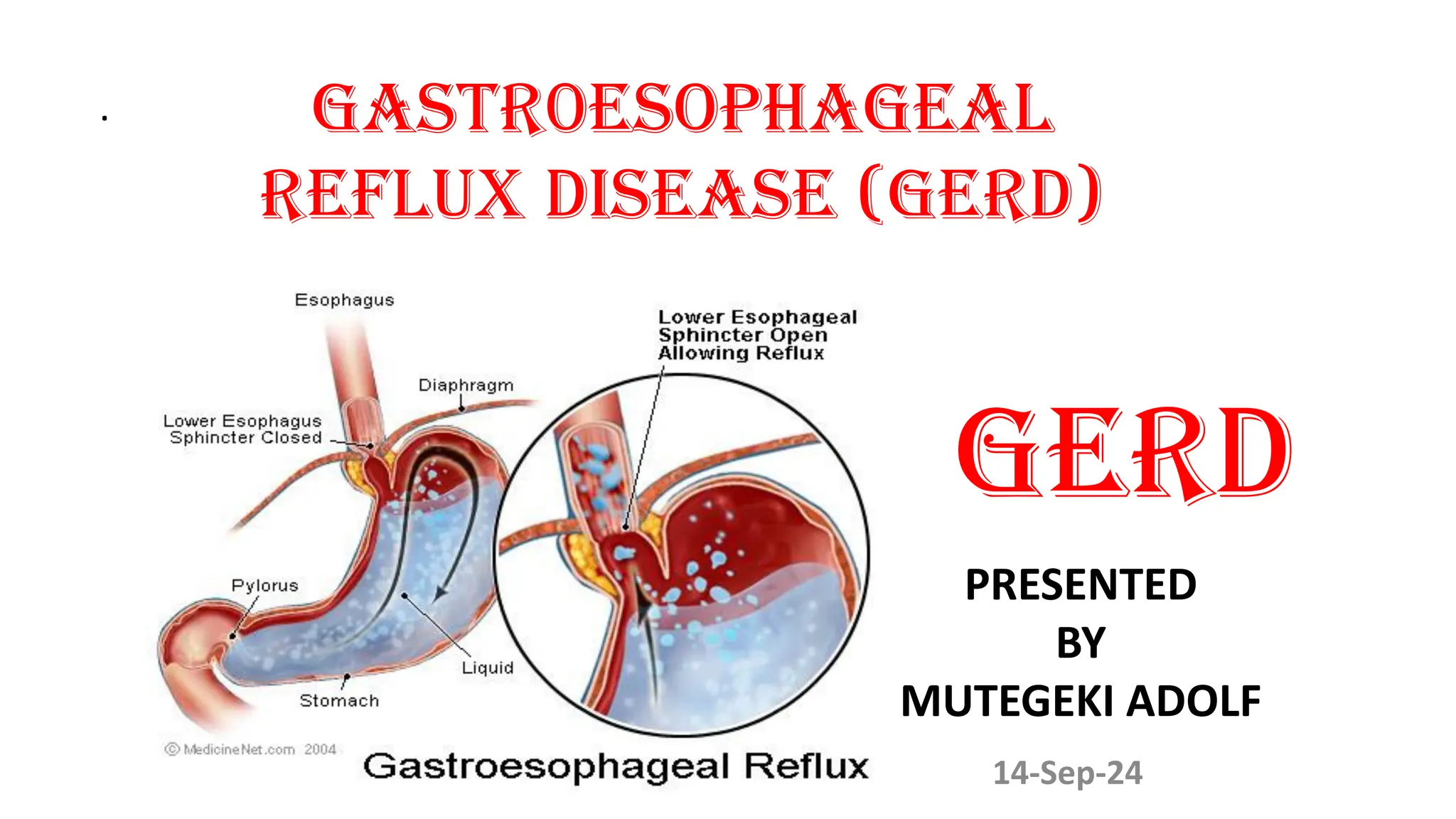
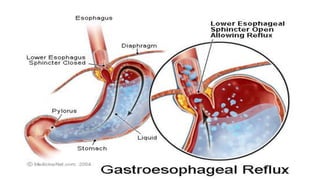
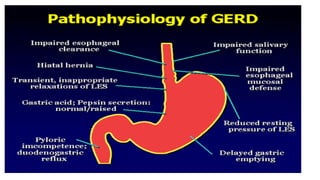
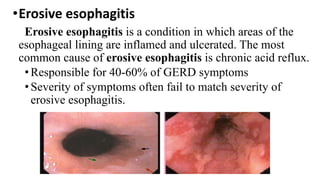
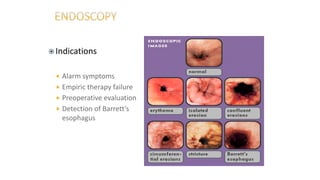
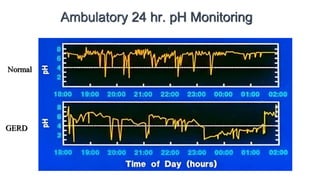
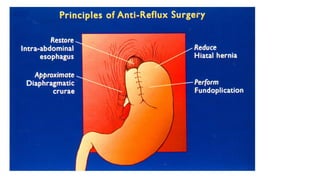
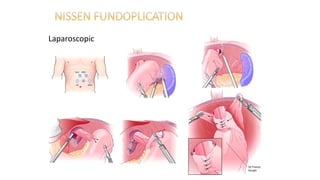
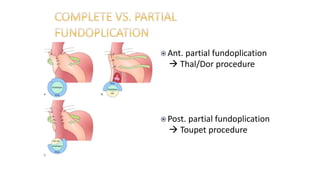
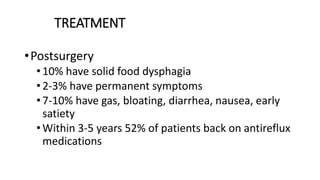
Gastroesophageal reflux disease (GERD) is a chronic condition where stomach contents reflux into the esophagus, primarily due to a weakened lower esophageal sphincter. It affects individuals of all ages but is most common in those over 40, with symptoms including heartburn, regurgitation, and difficulty swallowing. Treatment options include lifestyle modifications, medications such as antacids and proton pump inhibitors, and surgical interventions like fundoplication.