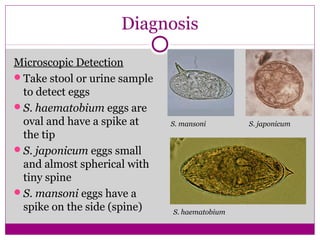
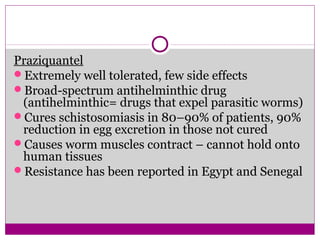
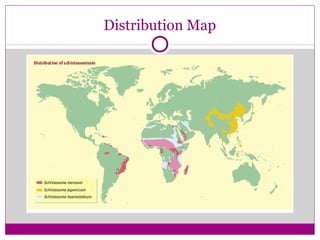
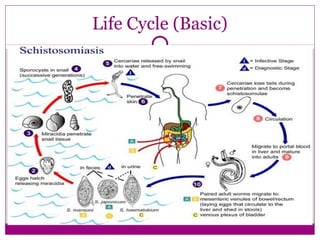
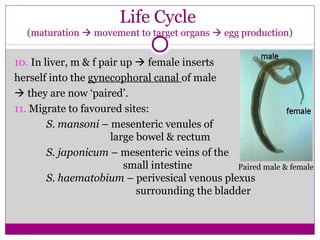
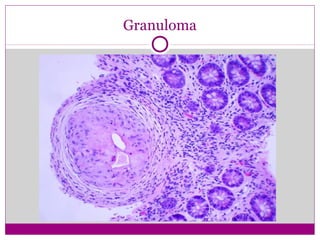
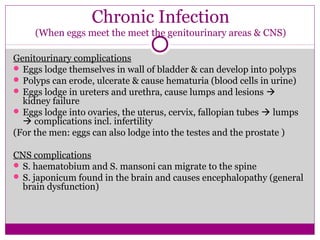
Schistosomiasis is a parasitic disease caused by several species of flatworm. It affects over 200 million people in developing countries. People can become infected by wading or swimming in freshwater bodies inhabited by snails that carry the parasite larvae. The parasite has a complex lifecycle involving snail and human hosts. In humans, the larvae mature into adult worms that reside in blood vessels and release eggs, which can cause immune reactions and organ damage. Symptoms range from rash and fever during initial infection to long-term issues like bladder polyps, kidney failure, and cancer. Diagnosis involves detecting parasite eggs in stool or urine samples, and treatment is usually with the drug praziquantel.






![ The commonest presentation is terminal haematuria [sometimes
uniform or microscopic]
Haematuria initially painless.
Burning micturation and hypogastric pain
Ureteric colic [due to the passage of coagulated blood from a
source of bleeding situated high up in the ureter]
Pain and burning sensation in the epigastrium- due to involvement
of the submucosa of the stomach
High urinary blood and protein levels are related to intensity of
infection and lower urinary tract pathology](https://image.slidesharecdn.com/schistosomiasis97031-160504142802/85/Genitourinary-Schistosomiasis-14-320.jpg)

![Carcinoma of bladder [squamous cell
type]](https://image.slidesharecdn.com/schistosomiasis97031-160504142802/85/Genitourinary-Schistosomiasis-16-320.jpg)