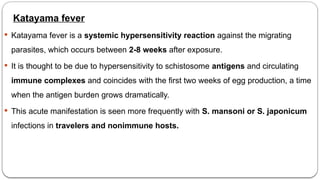
The document provides a comprehensive overview of schistosomiasis, a disease caused by parasitic blood flukes, affecting millions worldwide, particularly in tropical and subtropical regions. It details the epidemiology, various species, pathogenesis, clinical features, and treatment approaches, highlighting the significant health risks associated with the disease, including chronic infections and severe complications. Key symptoms vary by infection type and can include acute symptoms such as swimmer's itch and katayama fever, as well as chronic manifestations like abdominal pain and hepatomegaly.