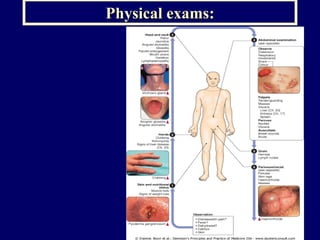
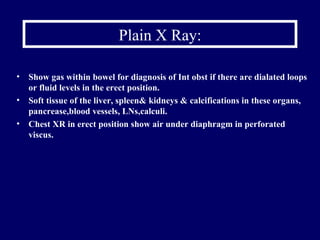
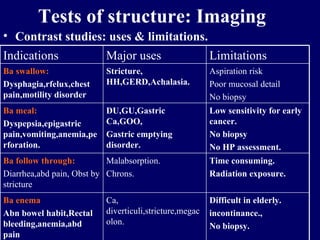
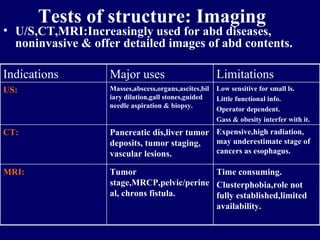
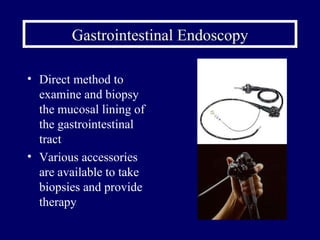
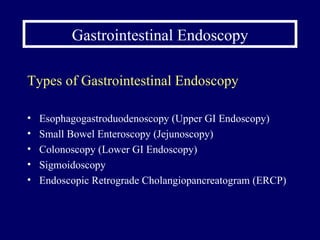
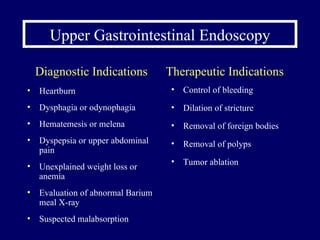
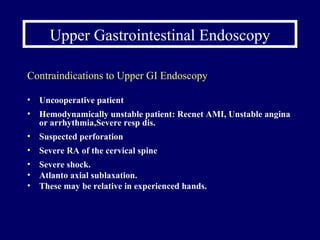
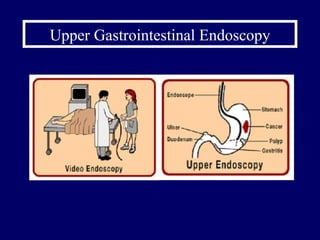
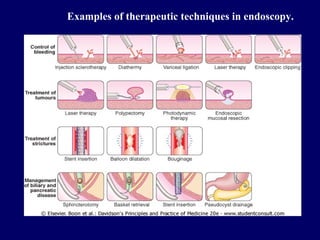
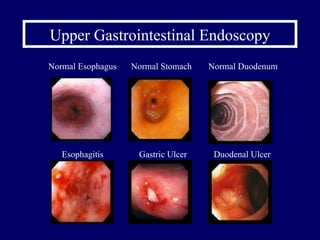
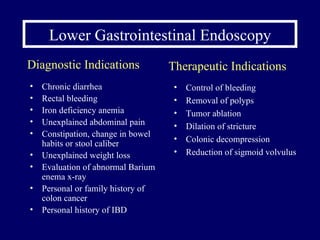
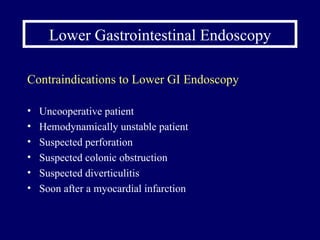
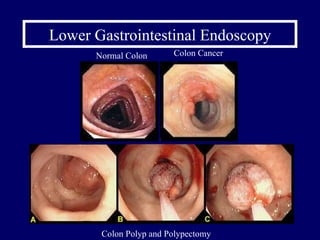
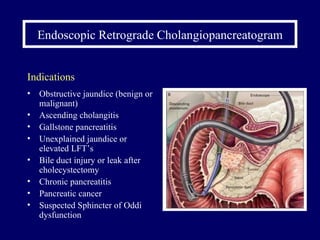
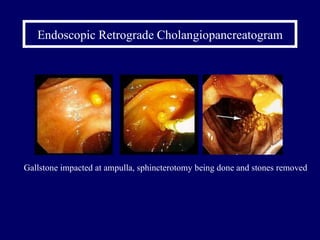
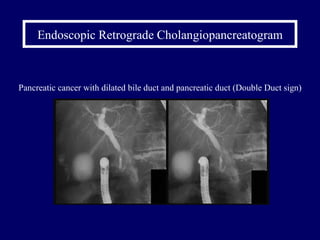
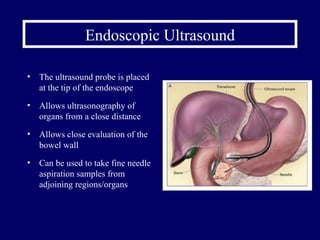
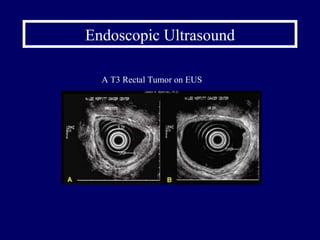
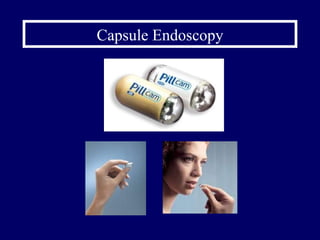
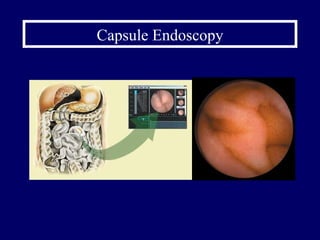
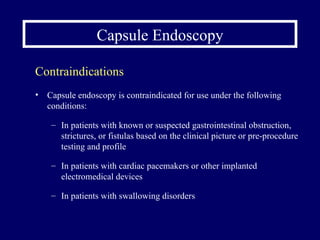
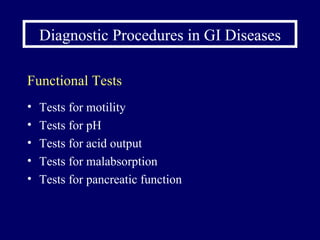
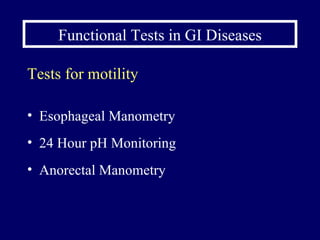
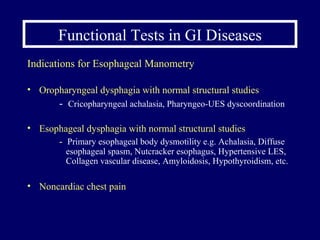
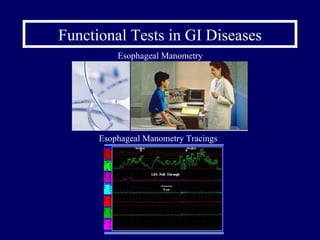
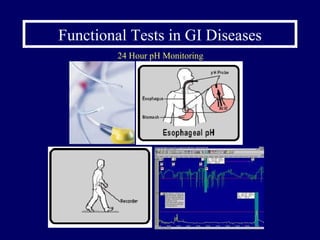
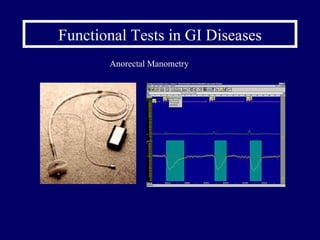
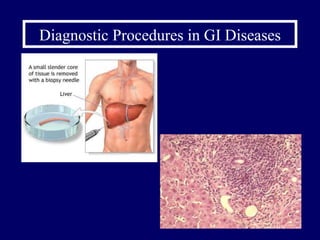
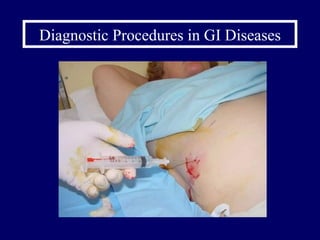
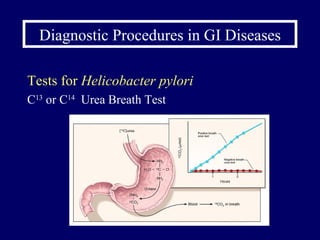
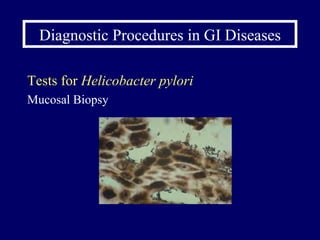
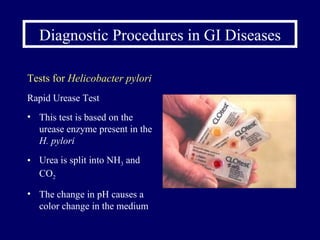
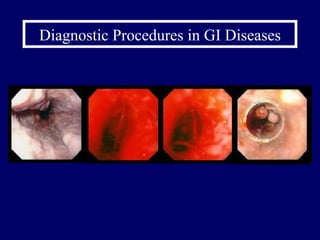
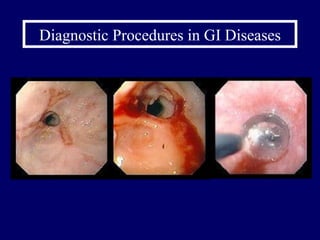
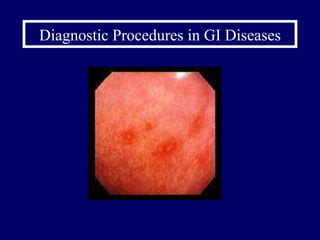
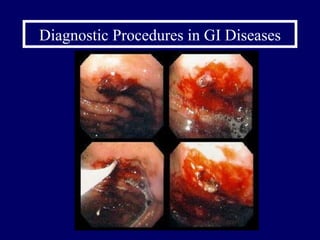
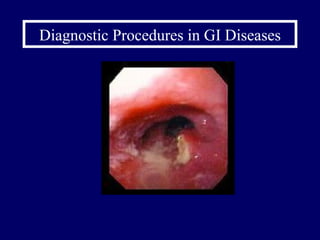
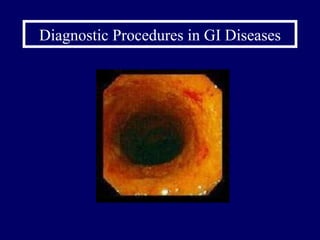
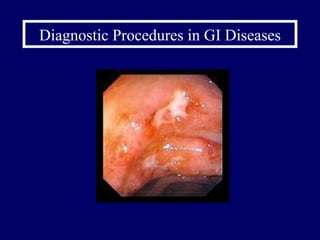
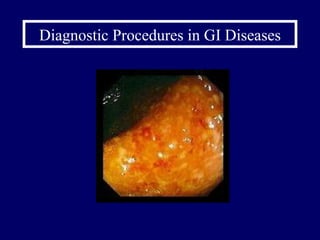
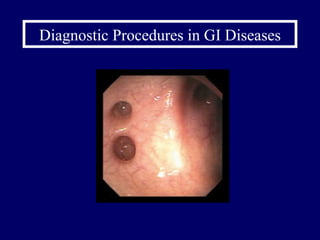
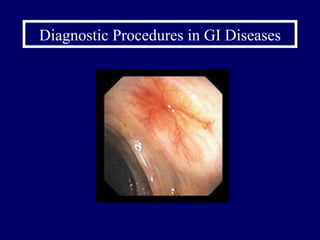
The document discusses various diagnostic procedures used in gastrointestinal (GIT) diseases. It describes structural tests like imaging techniques (X-rays, ultrasound, CT, MRI, endoscopy), functional tests (motility tests, pH monitoring, malabsorption tests), tests for infections like Helicobacter pylori, blood tests, and stool tests. Key diagnostic procedures mentioned include upper and lower endoscopy, capsule endoscopy, ERCP, EUS, biopsy, and hydrogen breath testing.