This document provides an overview of lower limb orthotics, including:
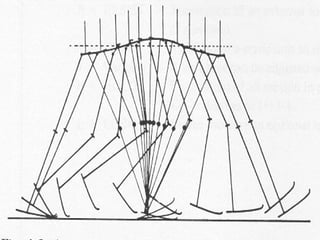
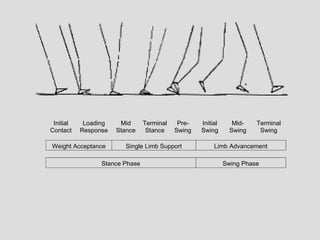
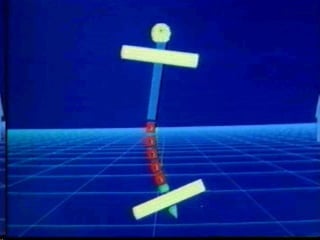
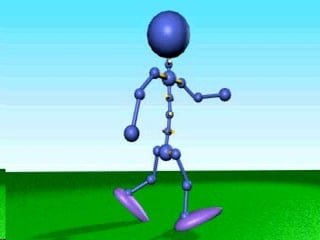
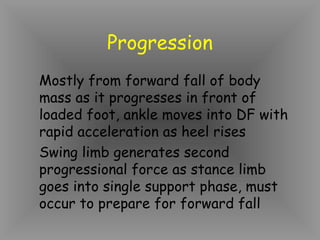
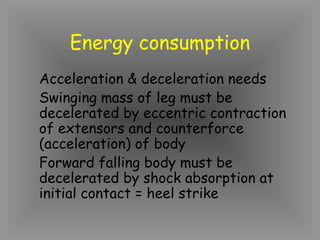
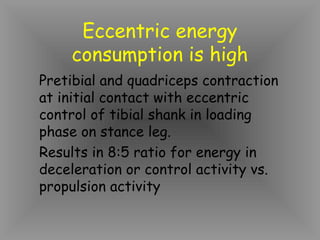
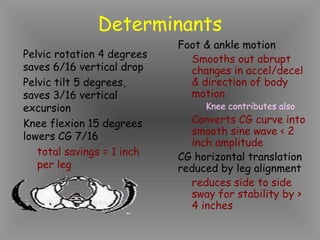
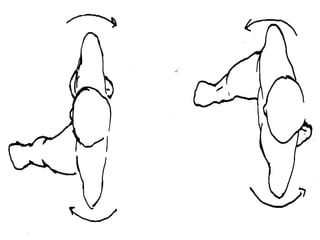
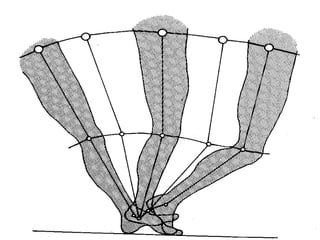
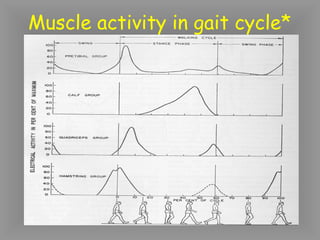
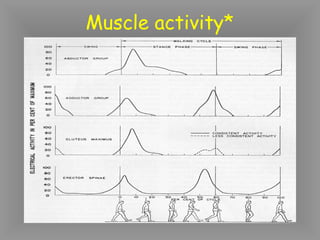
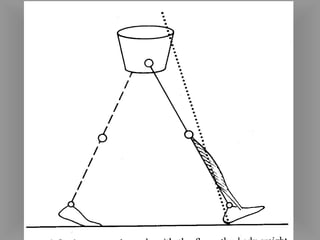
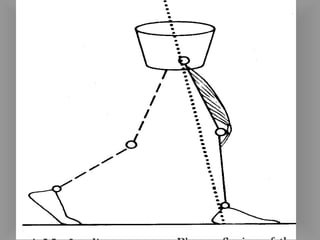
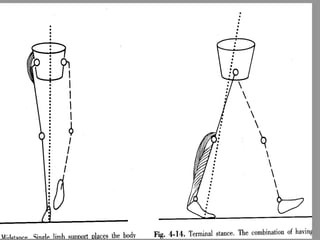
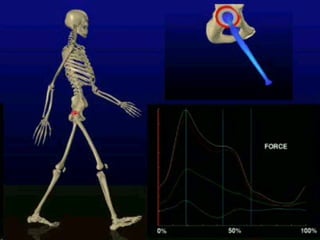
1. It describes normal gait mechanics and terminology used in gait analysis.
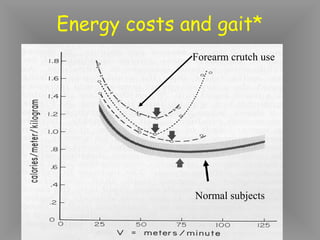
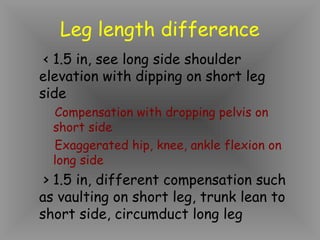
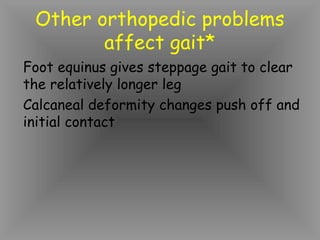
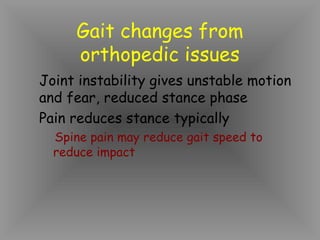
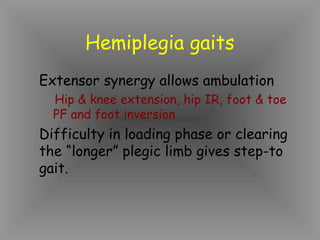
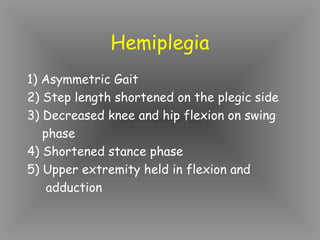
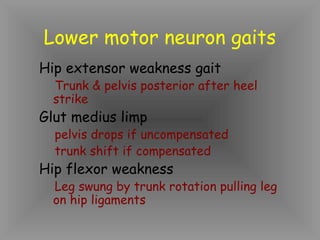
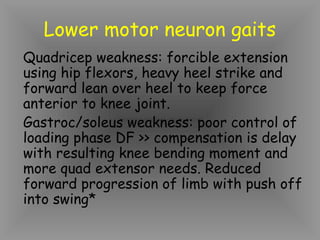
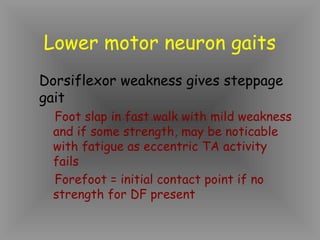
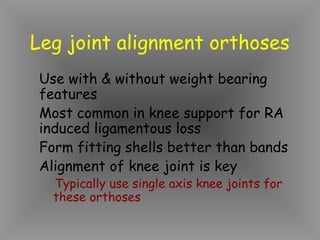
2. It discusses common orthopedic conditions that may require orthotics, such as leg length discrepancies, joint instability, and neurological impairments.
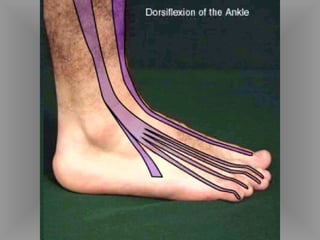
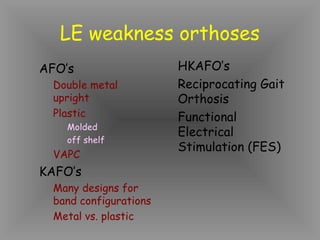
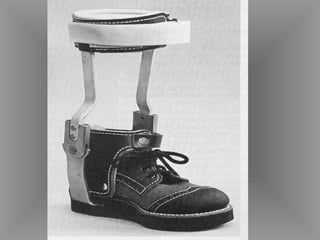
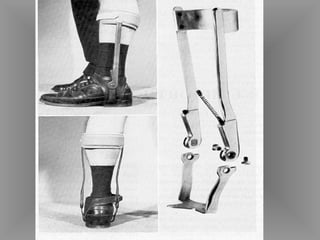
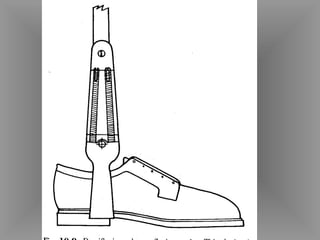
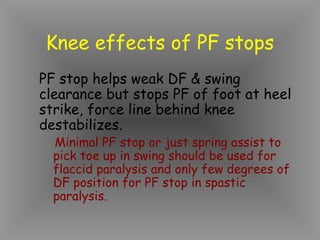
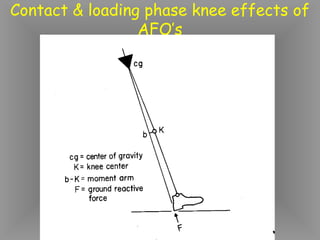
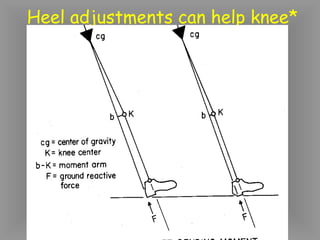
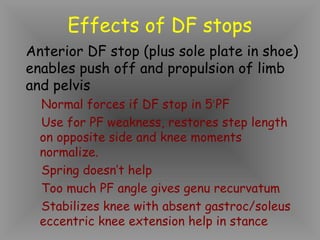
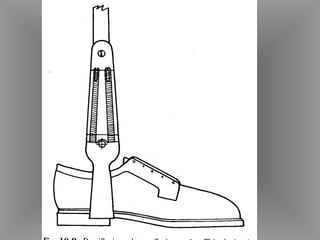
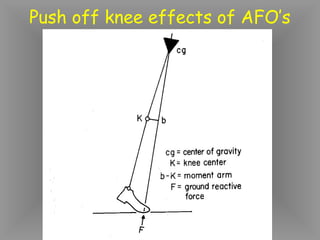
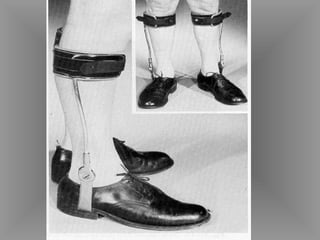
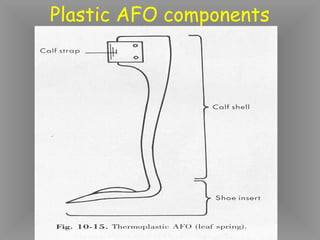
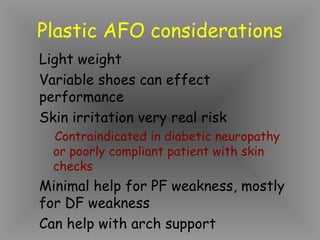
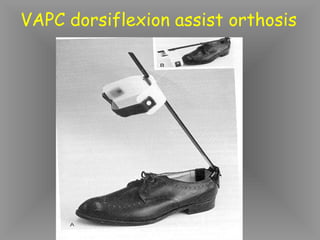
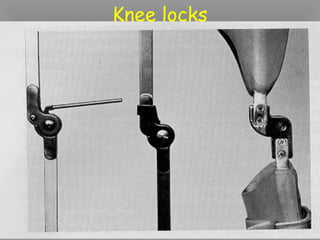
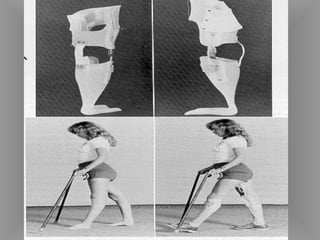
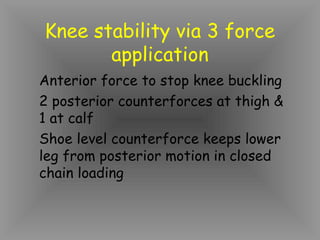
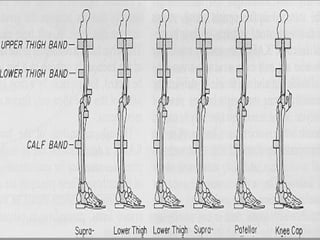
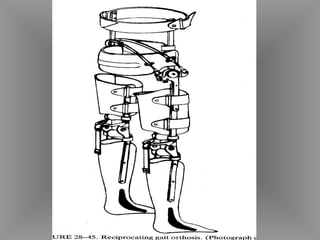
3. It explains different types of lower limb orthotics like AFOs, KAFOs, and knee orthoses, and how they can address weakness, alignment issues, and other impairments.