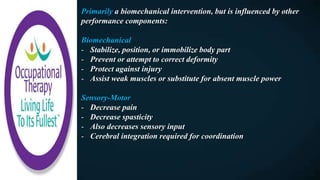
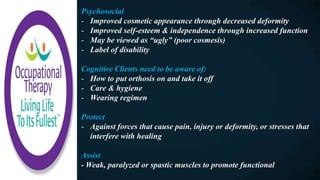
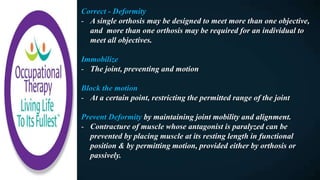
An orthosis is an externally applied device used to support the body, correct alignment, protect injuries, or assist motion. Occupational therapists play an important role in orthotic intervention by understanding orthotic goals, designs, and fitting to promote function. Common orthoses include those for the foot, ankle, knee, and upper limb to improve mobility and rehabilitation outcomes. Custom orthoses are fitted by orthotists/prosthetists while prefabricated devices may be fitted by other practitioners.



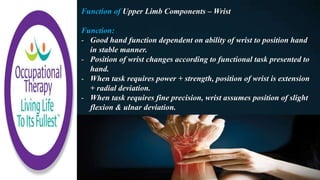
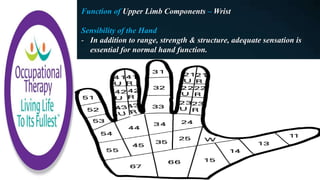
![The Wrist
The wrist will act as the keystone for hand positioning and outlines
the basis for all splinting, except isolated digital splinting.
The weight of the immobile hand, gravity, and resting muscle
tension tend to pull the wrist into flexion, which increases tension
in the extrinsic extensor tendons, pulling the metacarpophalangeal
(MCP) joints into hyperextension.
Concurrently, the tension of the extrinsic flexor is maintained
while forcing the interphalangeal (IP) joints (which include the
proximal interphalangeal [PIP] and distal interphalangeal [DIP]
joints) into flexion.
The metacarpal arch of the hand flattens and the thumb falls into
adduction. This results in a “claw hand” that is not functional.
Prevention of this deformity is one goal of hand splinting.](https://image.slidesharecdn.com/031-180730003124/85/Occupational-Therapy-and-Orthotic-Intervention-15-320.jpg)