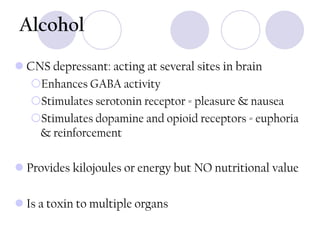
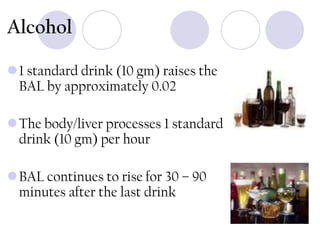
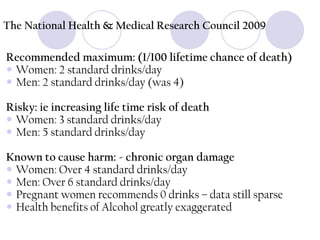
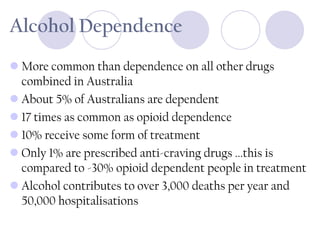
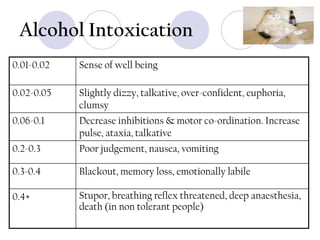
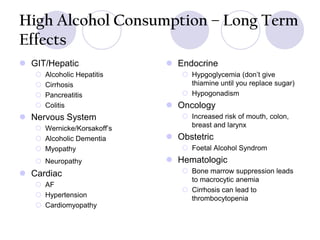
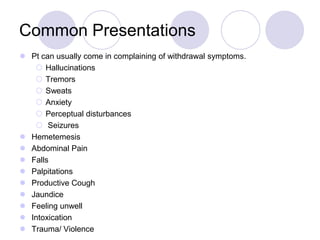
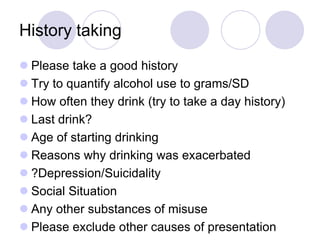
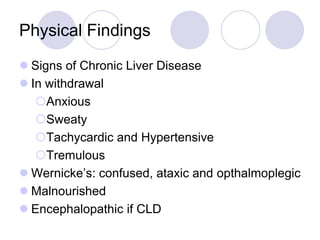
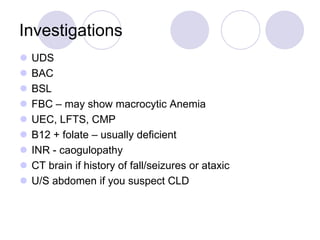
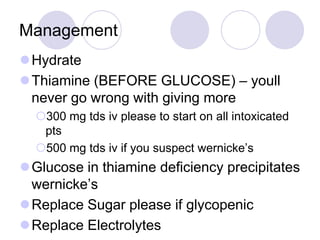
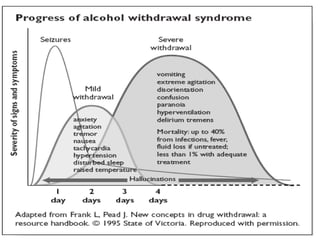
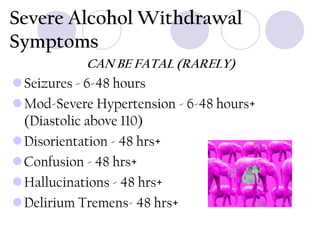
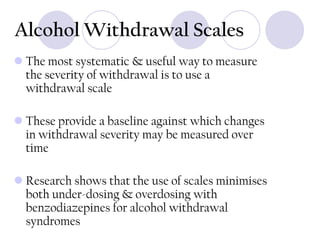
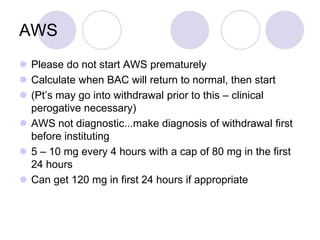
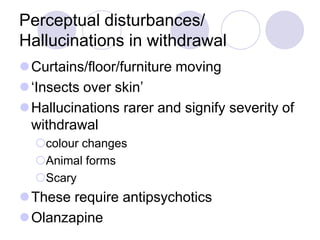
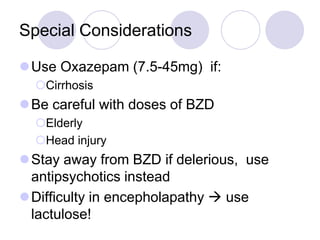
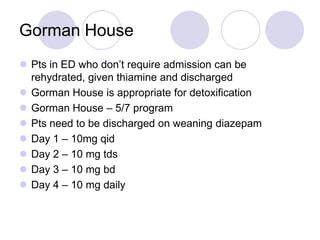
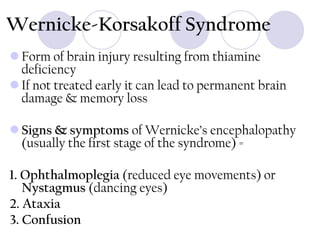
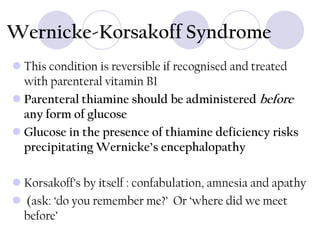
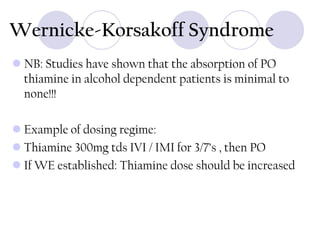
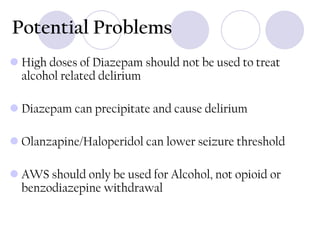
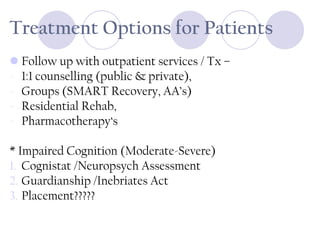
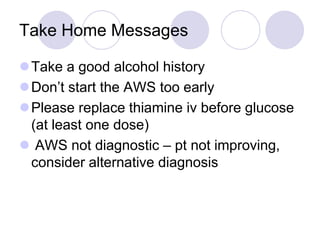
This document provides information on alcohol, its effects on the body, alcohol dependence and withdrawal, and treatment approaches. It discusses how alcohol acts in the brain to produce both pleasurable and reinforcing effects. It outlines recommended daily and weekly drinking limits, signs and symptoms of alcohol intoxication at different blood alcohol levels. It also summarizes common presentations to the emergency department related to alcohol, approaches to assessing and managing alcohol withdrawal, risks of Wernicke's encephalopathy from thiamine deficiency, and options for ongoing treatment and support.