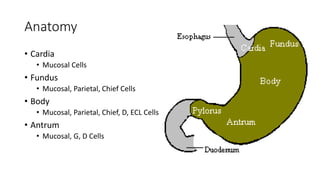
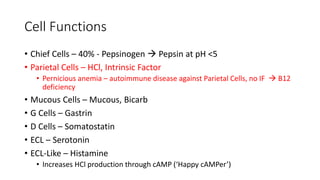
1. The stomach has several cell types that secrete different substances like pepsinogen, HCl, intrinsic factor, mucus, gastrin, and somatostatin. Diseases can affect these cells and their secretions.
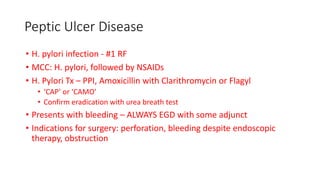
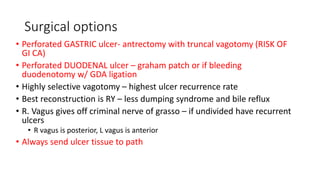
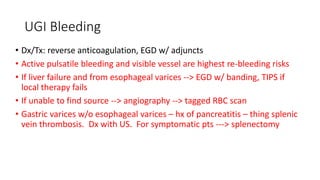
2. Common causes of peptic ulcer disease include H. pylori infection and NSAID use. Treatment involves eradicating H. pylori and managing risk factors. Surgery may be needed for complications like bleeding or perforation.
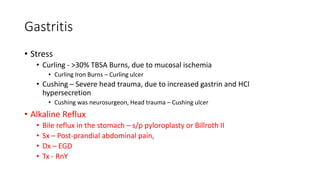
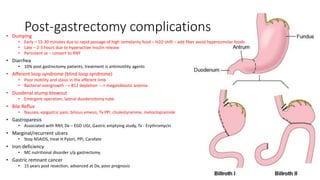
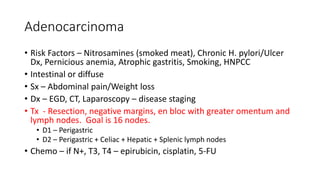
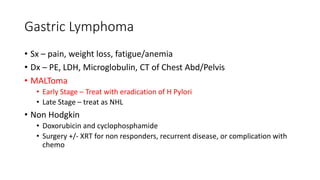
3. Other diseases discussed include gastritis, gastric cancer, GIST tumors, dumping syndrome, and lymphomas. Diagnosis involves endoscopy, imaging, and biopsies. Treatment depends on the specific disease but