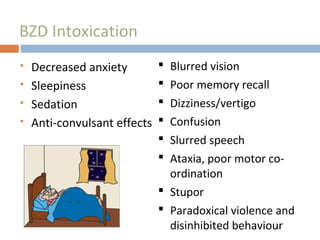
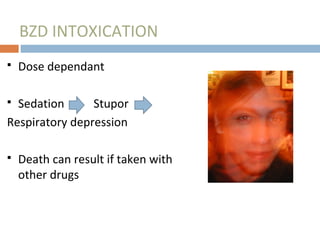
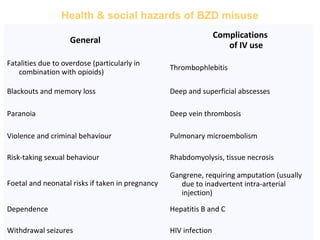
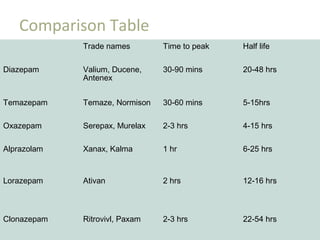
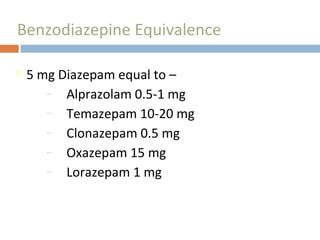
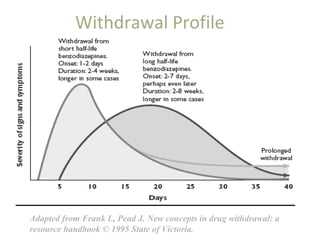
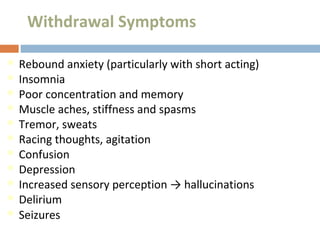
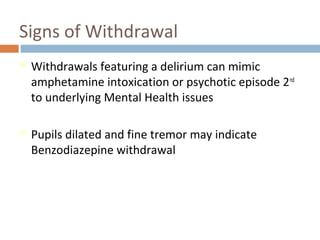
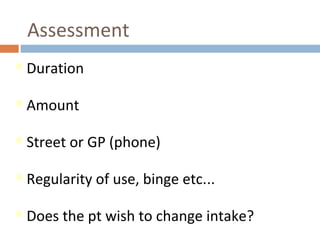
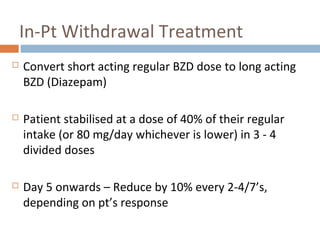
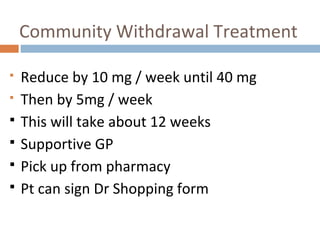
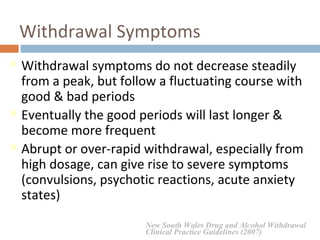
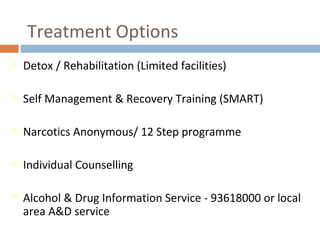
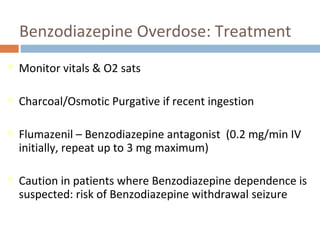
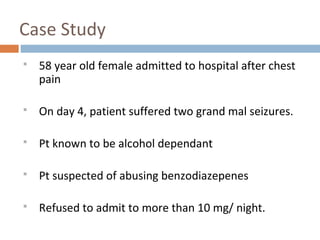
The document discusses benzodiazepines, including their uses, effects, risks of dependence and withdrawal, assessment and treatment of withdrawal, and overdose management. Benzodiazepines are widely used to treat anxiety, insomnia, and other conditions but can cause dependence, and withdrawal symptoms may include rebound anxiety, insomnia, tremors, and potentially seizures. Detoxification and tapering regimens aim to safely reduce the dose over time to minimize withdrawal symptoms.