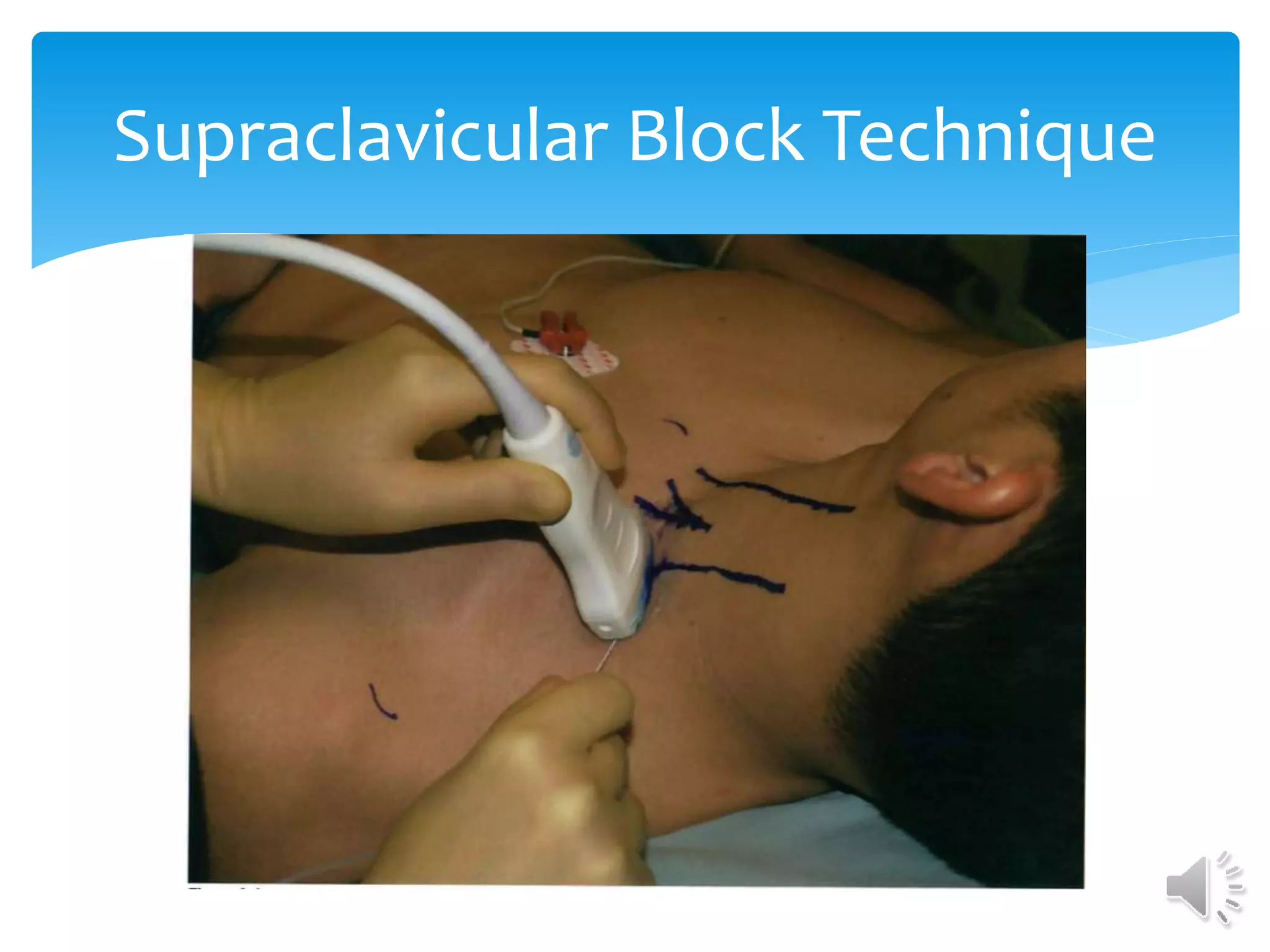
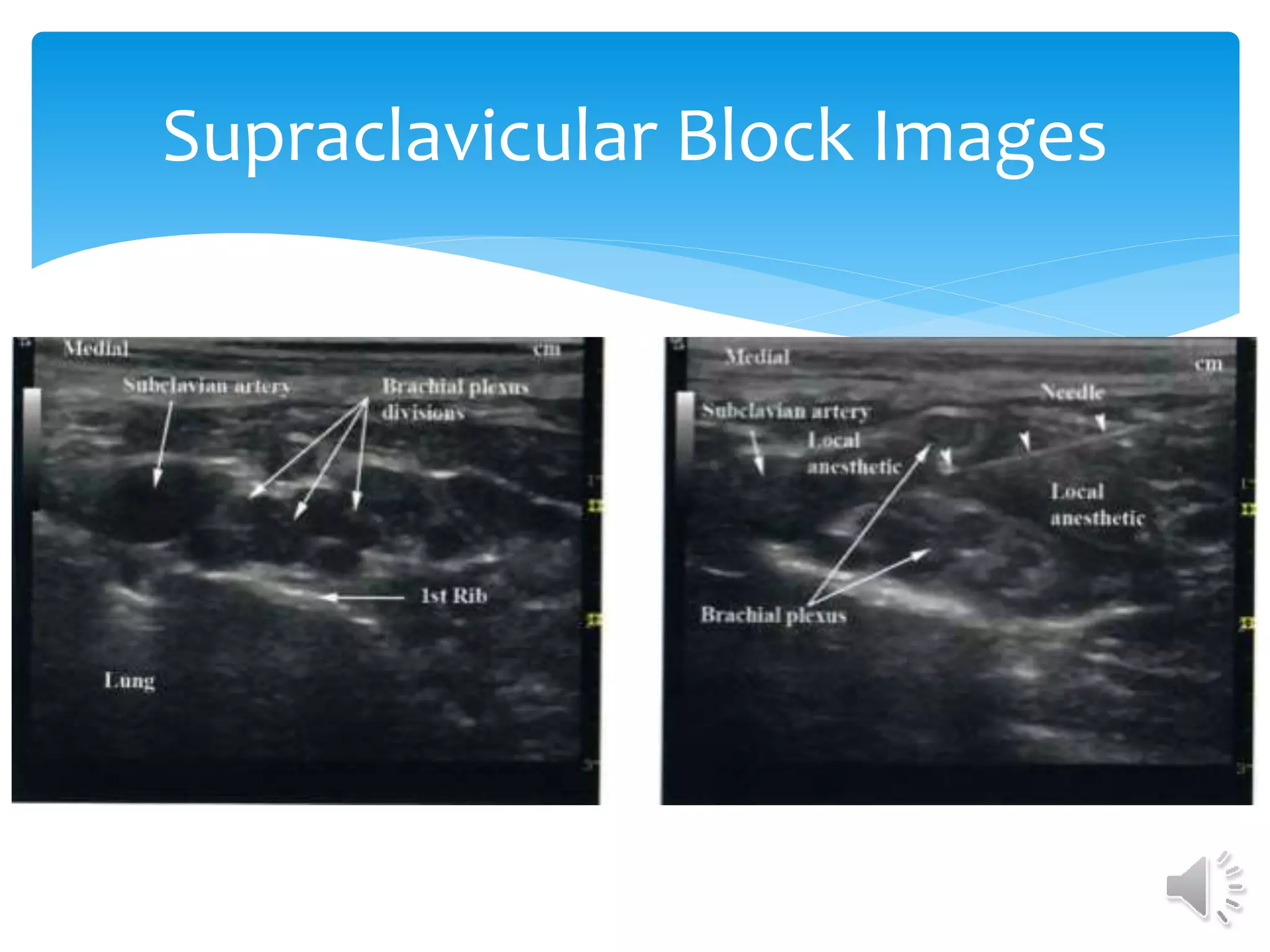
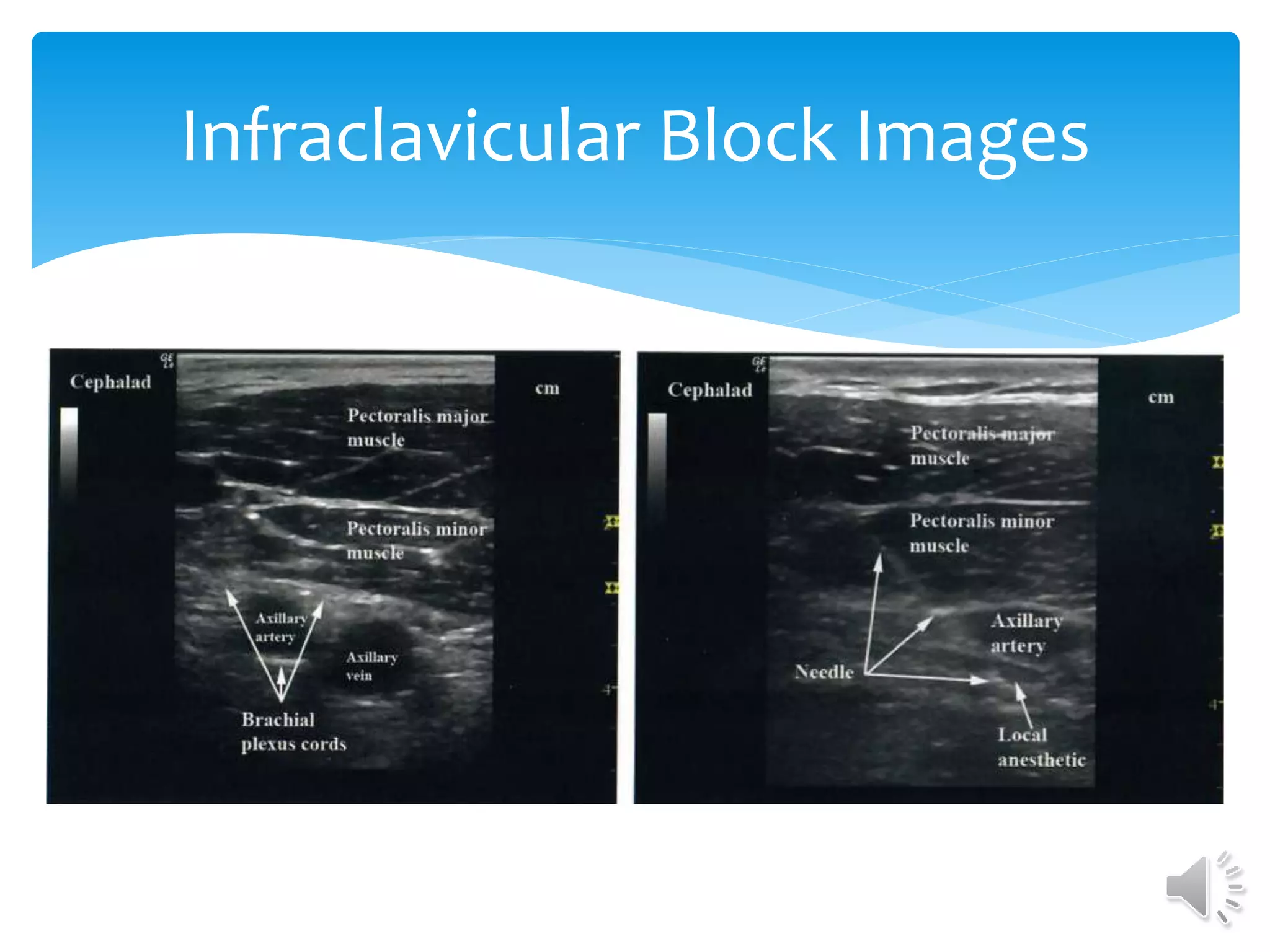
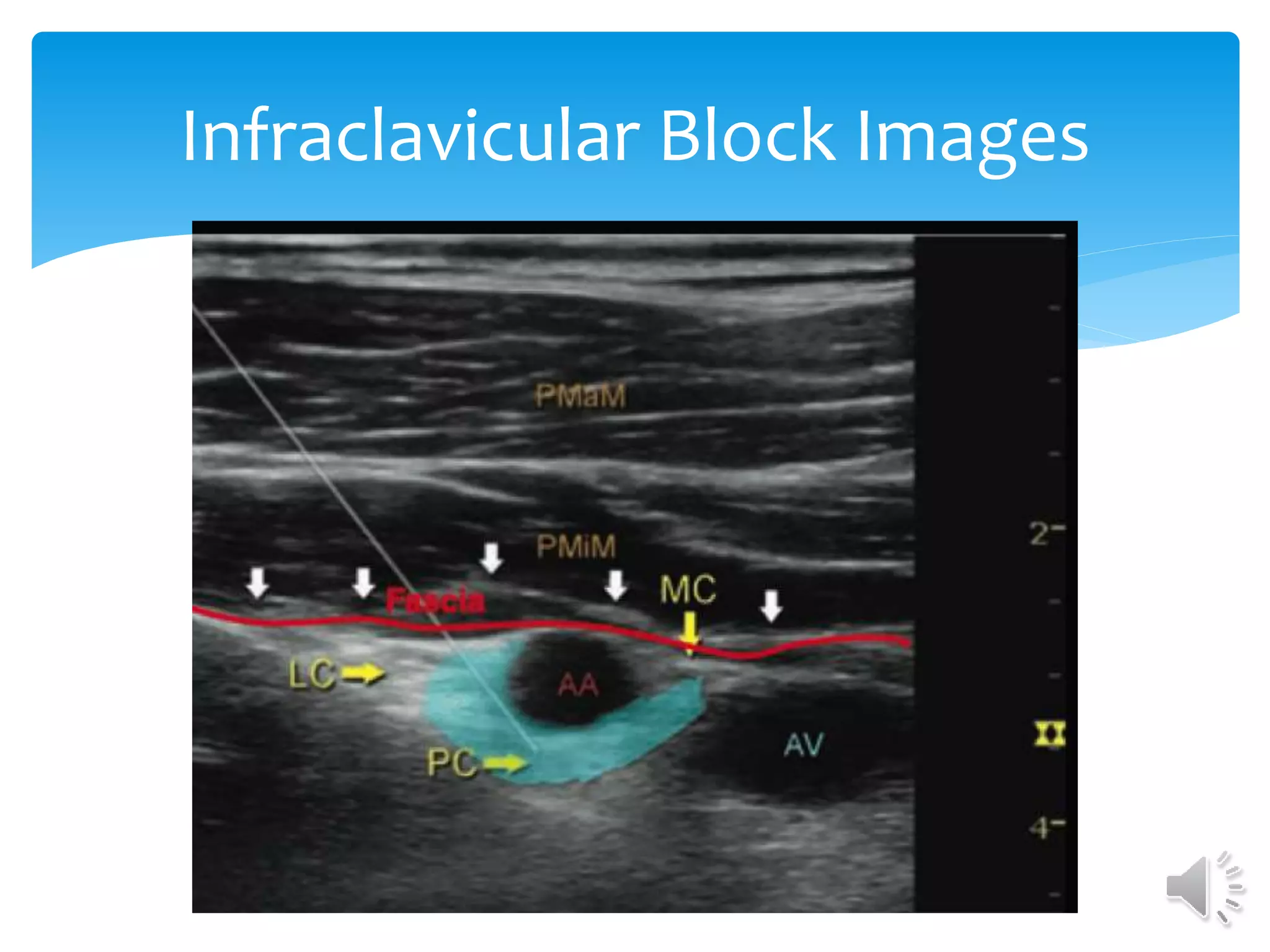
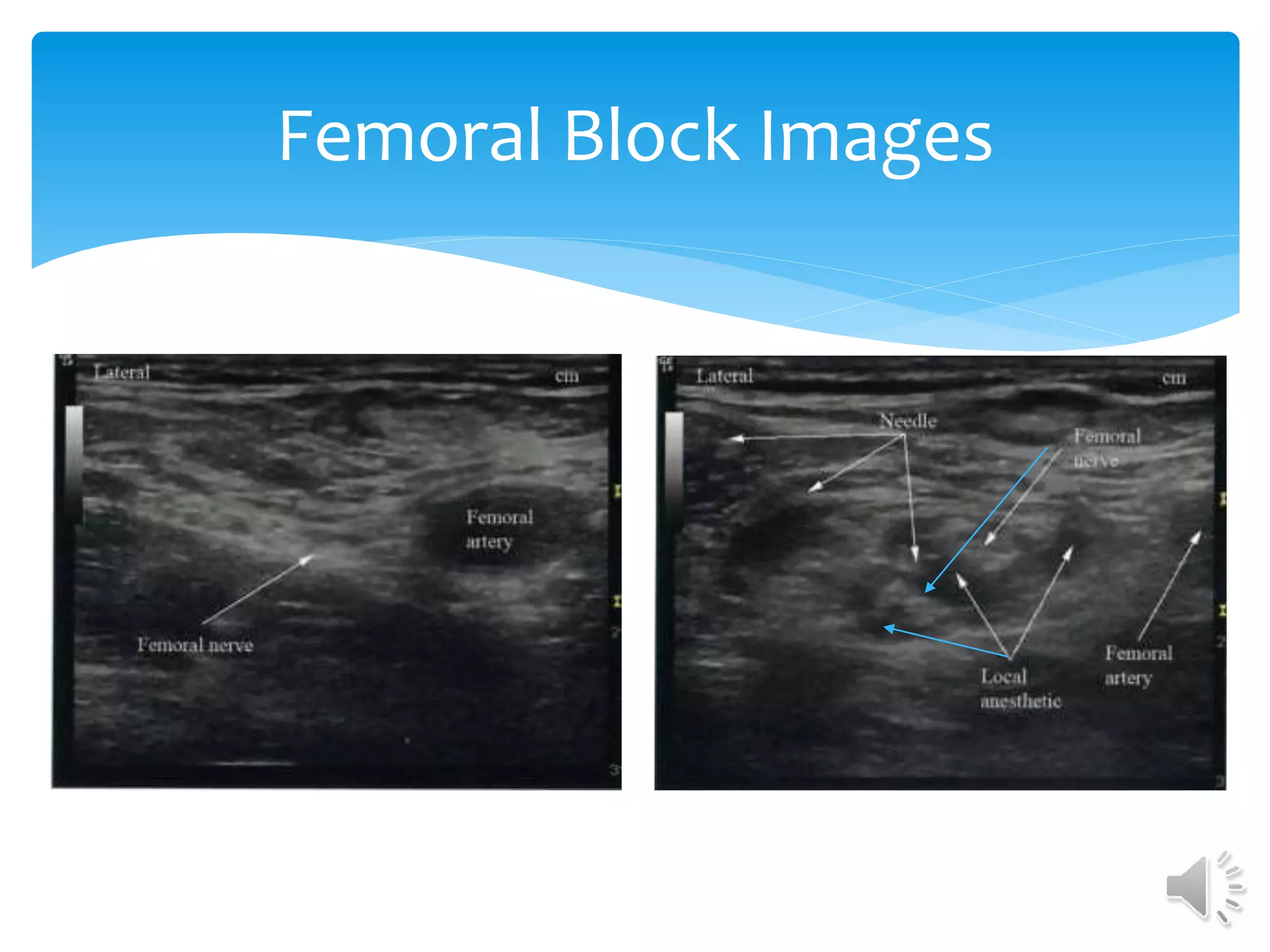
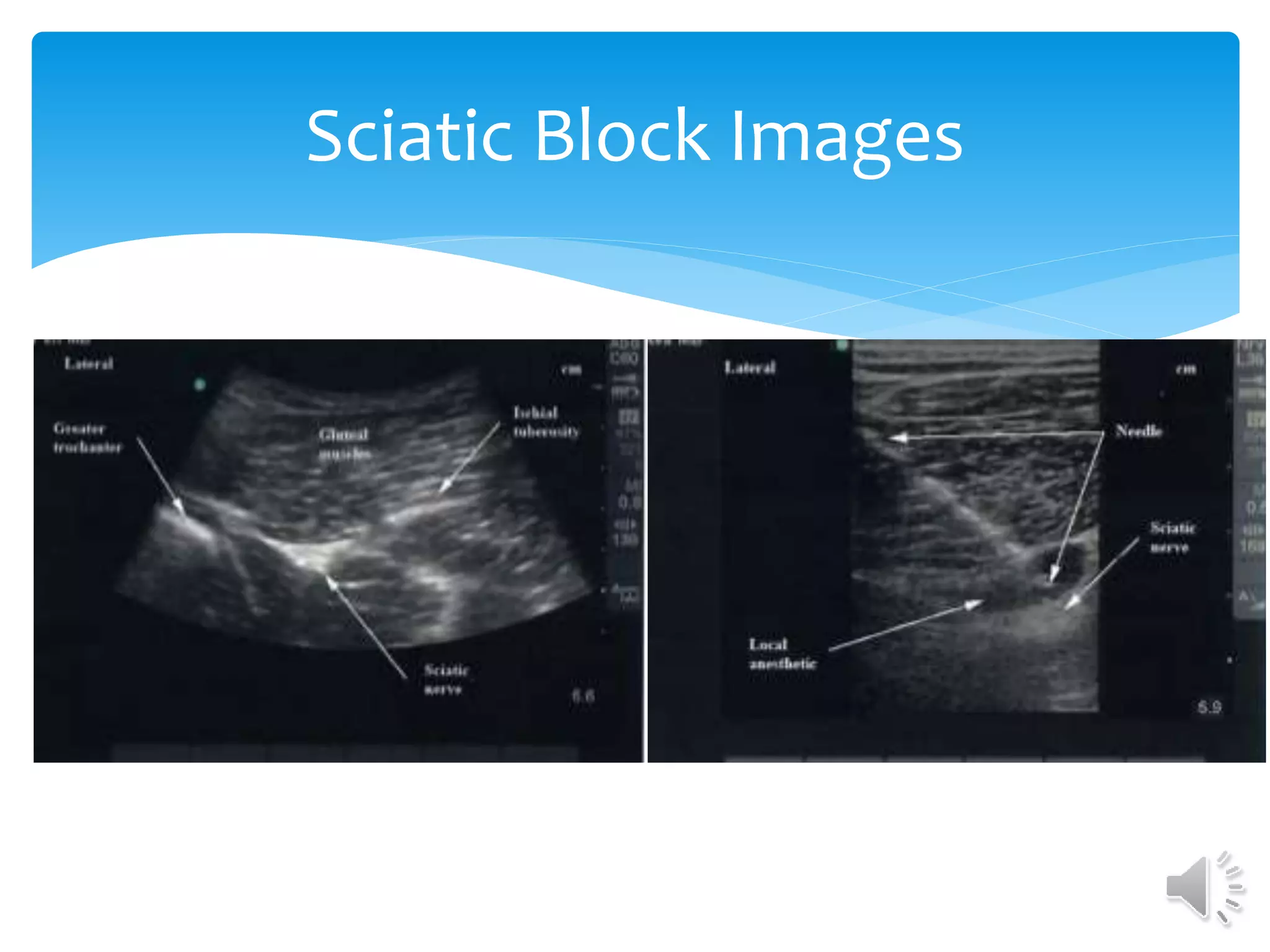
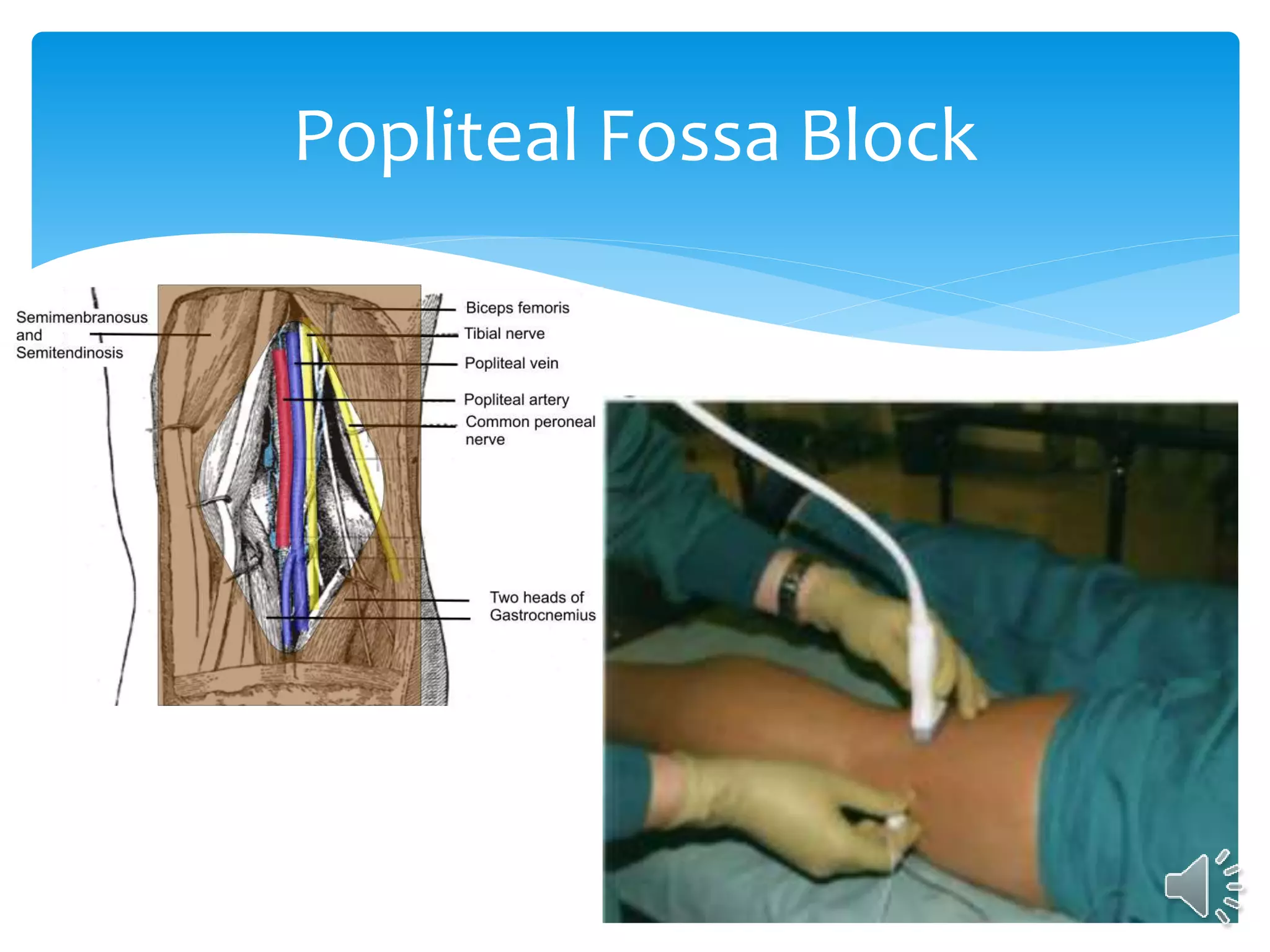
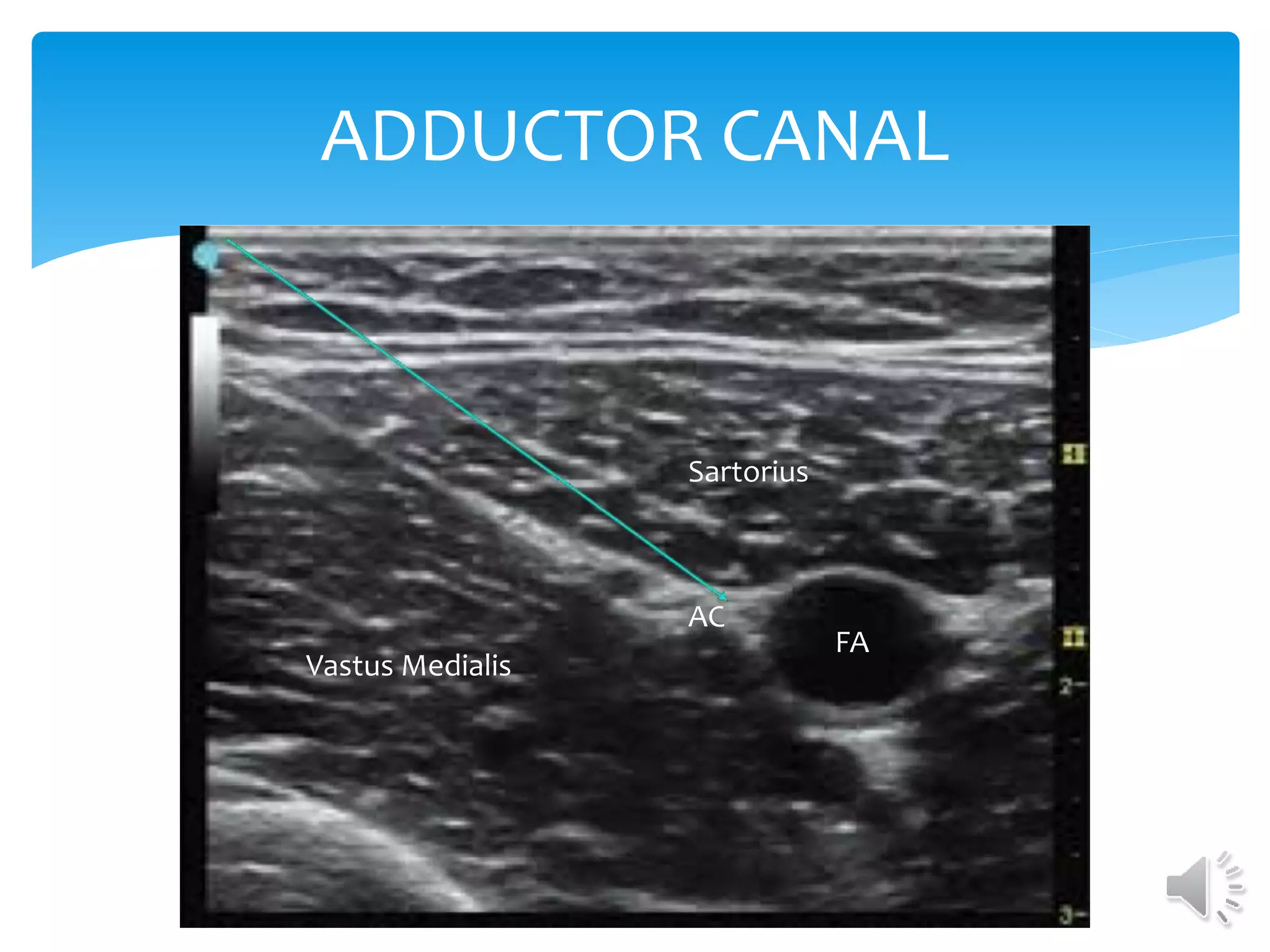
This document provides an overview of ultrasound-guided peripheral nerve blocks. It lists the benefits of ultrasound guidance such as visualizing surrounding structures and avoiding injury. It discusses machine controls and how to optimize ultrasound imaging. The objectives are to list benefits of ultrasound guidance, discuss machine controls, and identify images of peripheral nerves. It then covers techniques for various upper and lower extremity nerve blocks and provides ultrasound images of relevant anatomy.





















![References
Beaussier, M., Sciard, D., & Sautet, A. (2016). New modalities of pain treatment after
outpatient orthopaedic surgery. Orthopaedics & Traumatology, Surgery & Research :
OTSR, 102(1 Suppl), S121-4. doi:10.1016/j.otsr.2015.05.011 [doi]
Buckenmaier, C., & Bleckner, L. (2009). In Redding J. (Ed.), Military advanced regional
anesthesia and analgesia, handbook (First ed.). Washington, DC: Office of the Surgeon
General at TMM Publications.
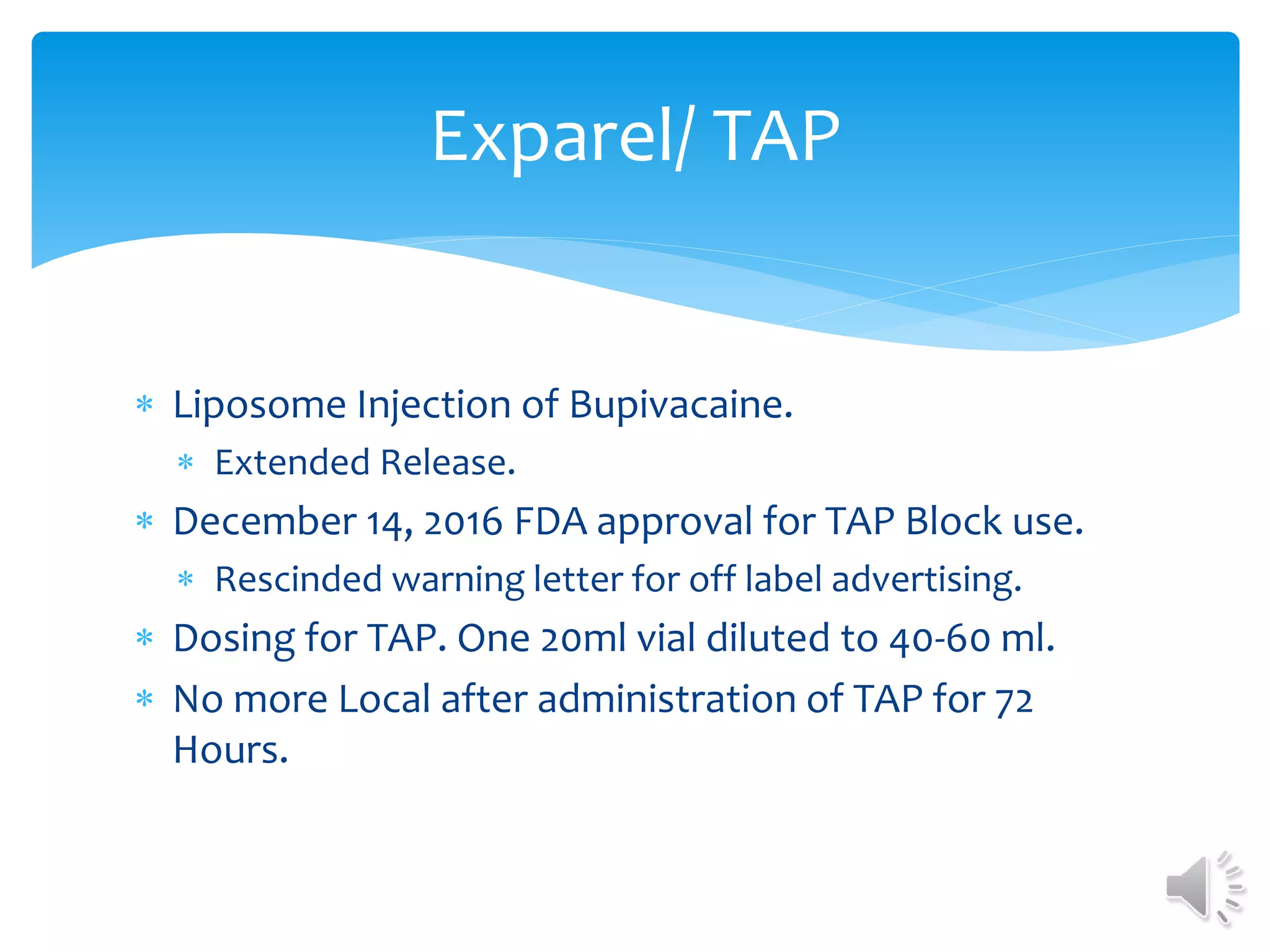
Food and Drug Administration. (2015). Removal of warning letter; TAP block approval.
Retrieved from
http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Enfo
rcementActivitiesbyFDA/WarningLettersandNoticeofViolationLetterstoPharmaceuticalC
ompanies/UCM477250.pdf
Lin, E., Choi, J., & Hadzic, A. (2013). Peripheral nerve blocks for outpatient surgery:
Evidence-based indications. Current Opinion in Anaesthesiology, 26(4), 467-474.
doi:10.1097/ACO.0b013e328362baa4 [doi]
Patacsil, J. A., McAuliffe, M. S., Feyh, L. S., & Sigmon, L. L. (2016). Local anesthetic
adjuvants providing the longest duration of analgesia for single-injection peripheral
nerve blocks in orthopedic surgery: A literature review. American Association of Nurse
Anesthetists Journal, 84(2), 95.](https://image.slidesharecdn.com/mcvickerncana1029-161107161806/75/Fundamentals-of-Ultrasound-Guided-Peripheral-Regional-Anesthesia-Techniques-47-2048.jpg)