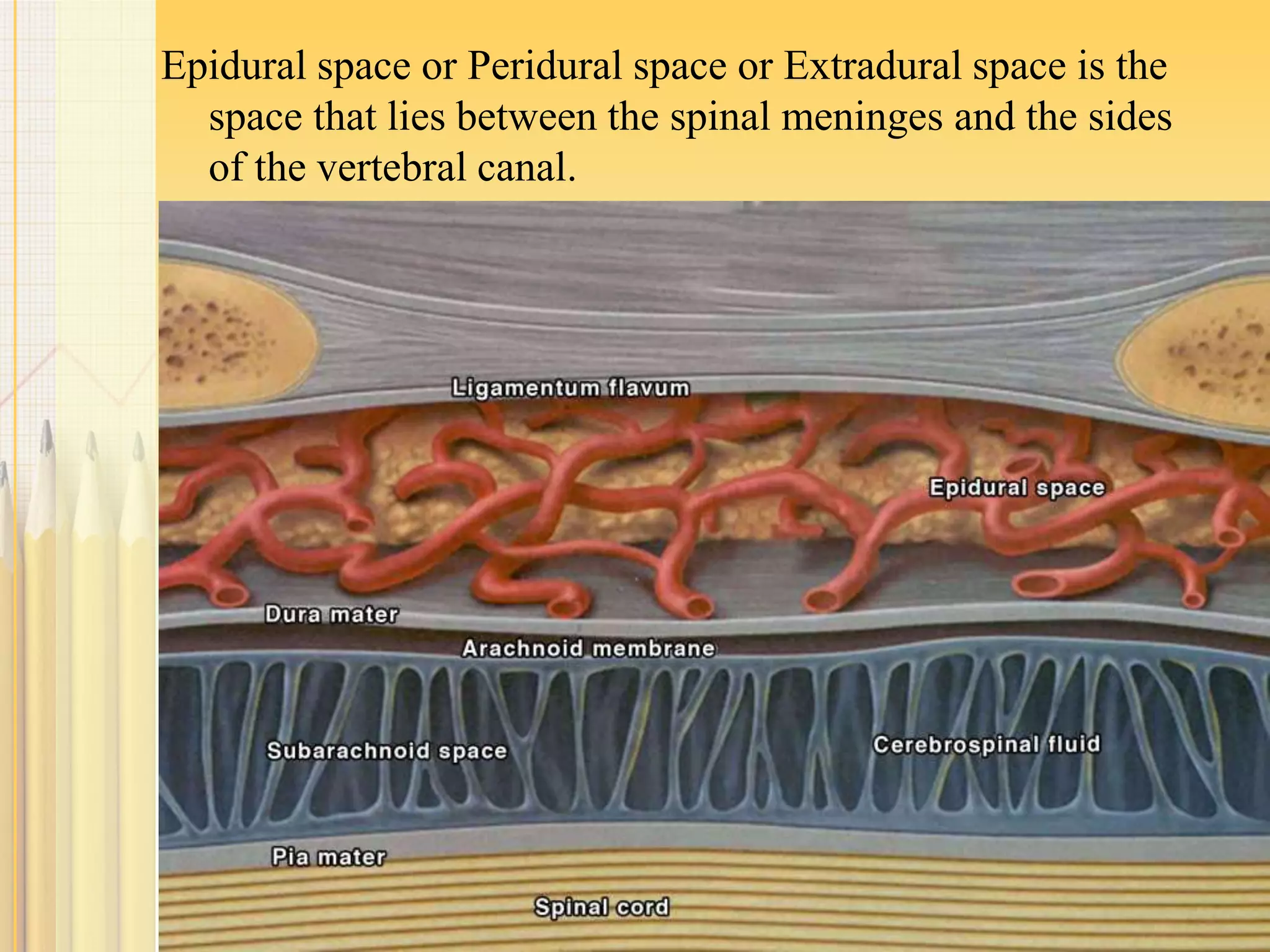
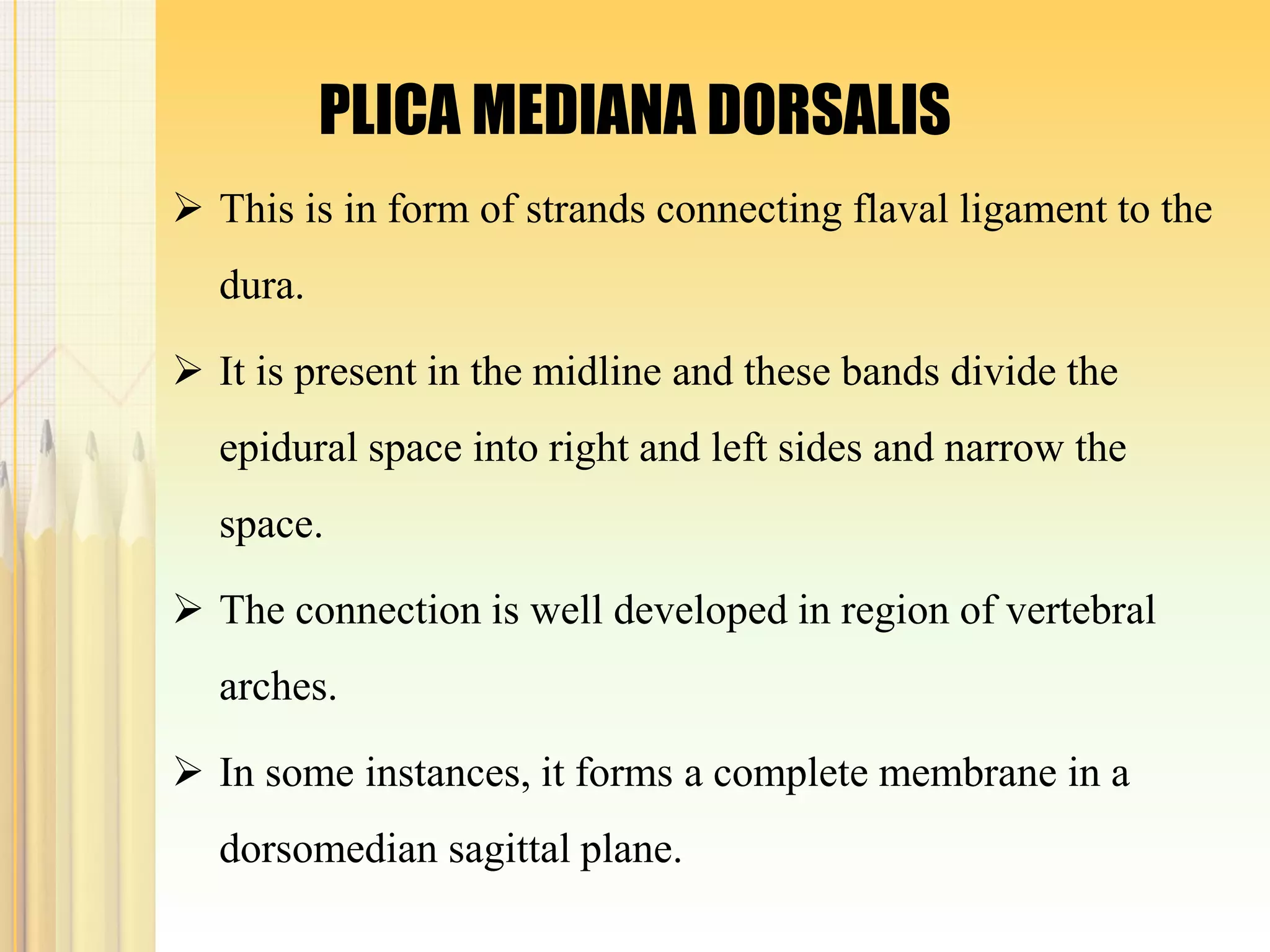
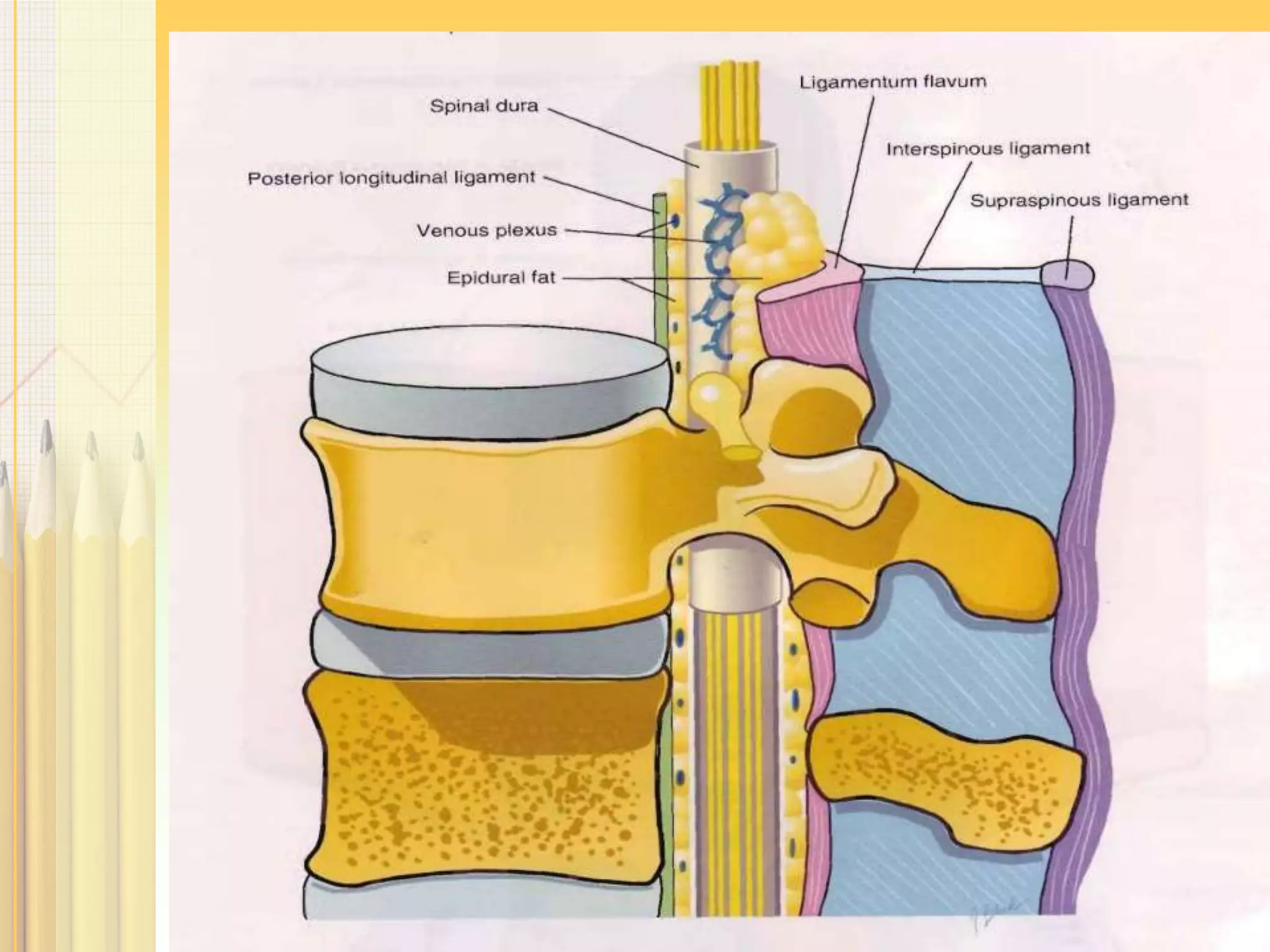
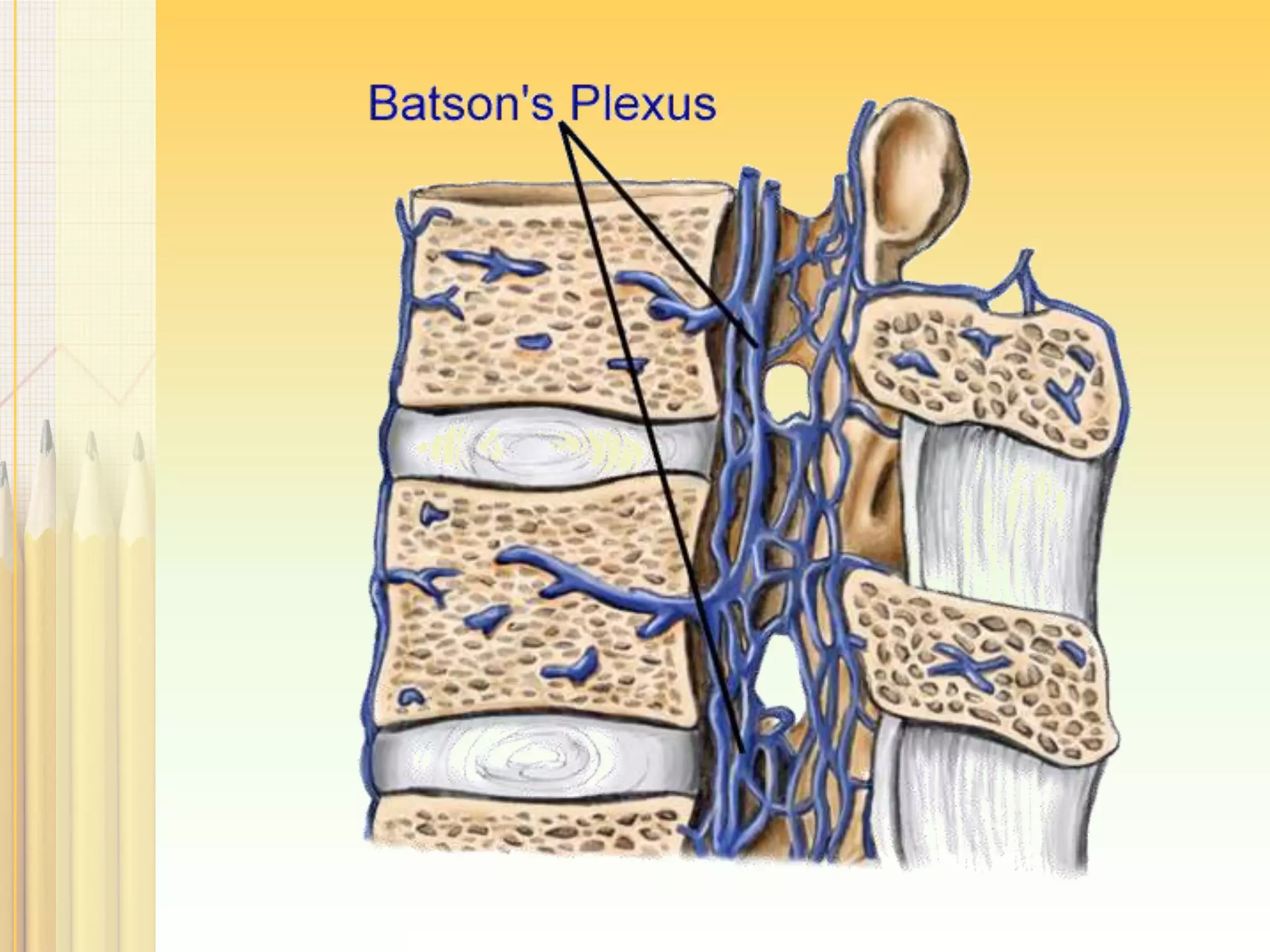
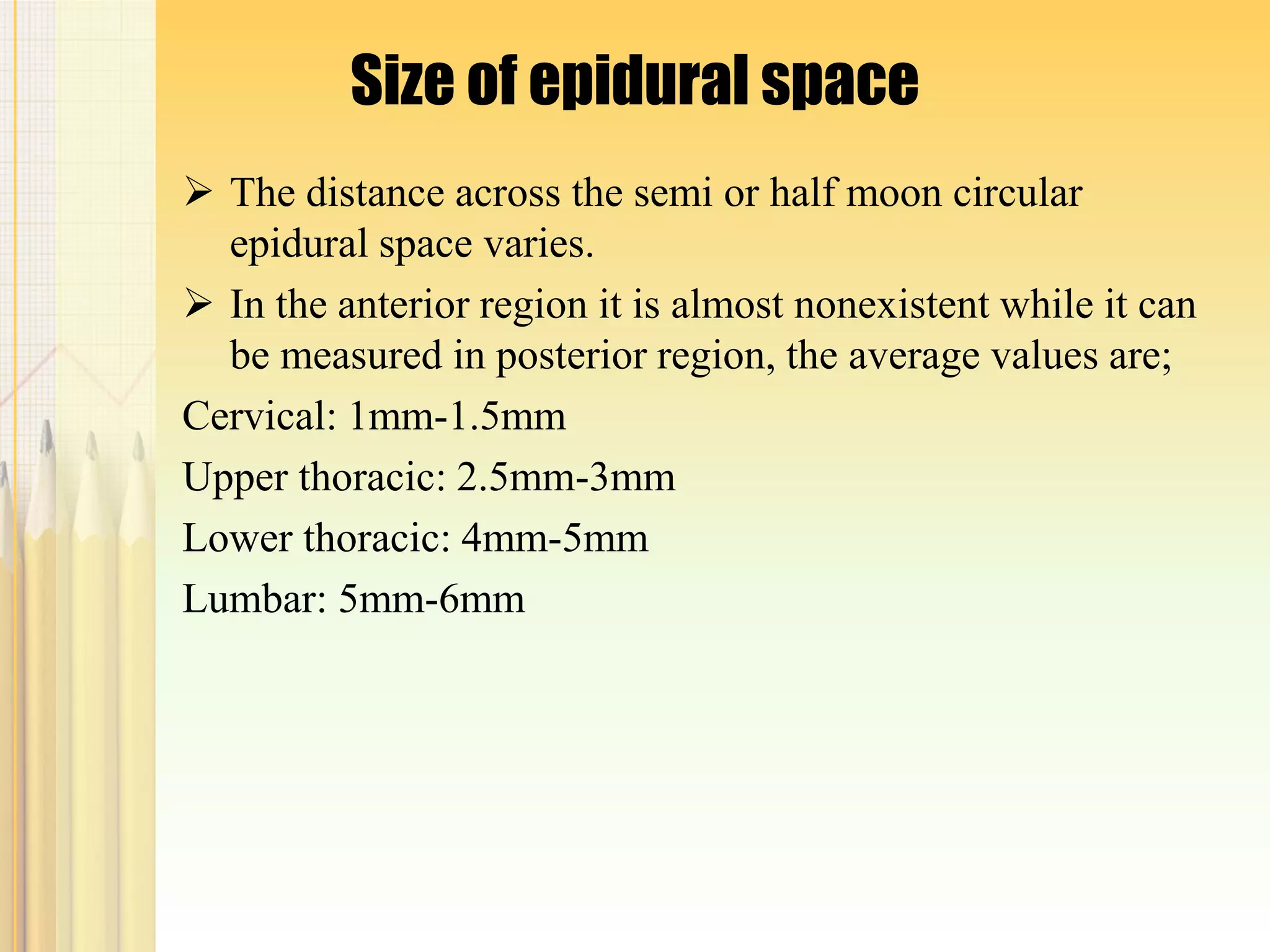
This document provides an overview of the anatomy of the epidural space. It discusses the boundaries, contents, size, and structures that must be penetrated to access the epidural space. Key points include that the epidural space lies between the spinal meninges and vertebral canal, contains connective tissue, fat, blood vessels and spinal nerves. It varies in size from 1-6mm depending on the spinal region. To access it requires penetrating the skin, ligaments and ligamentum flavum in the midline.