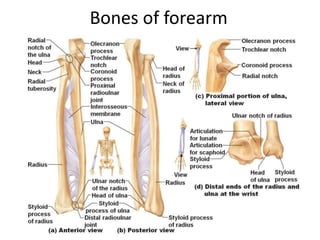
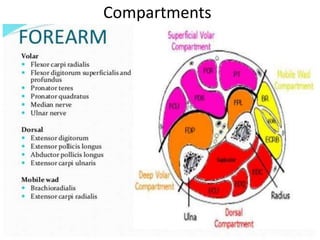
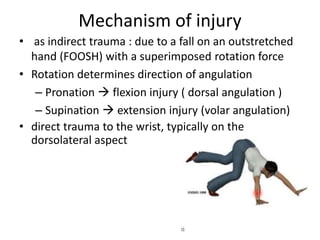
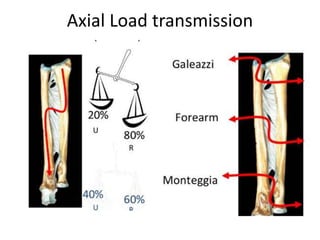
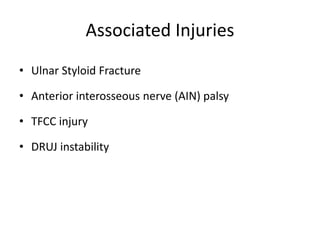
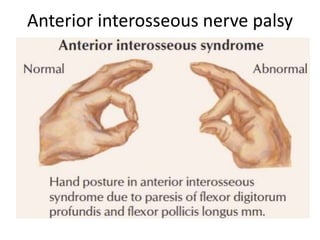
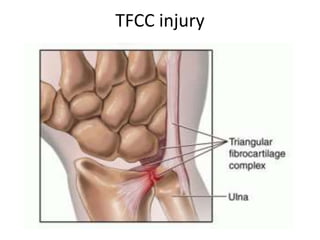
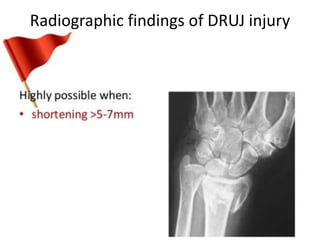
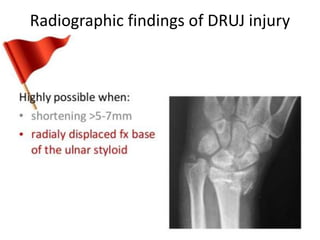
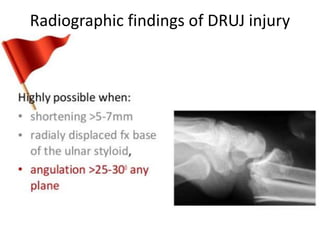
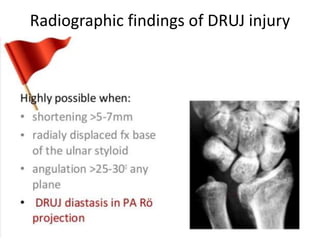
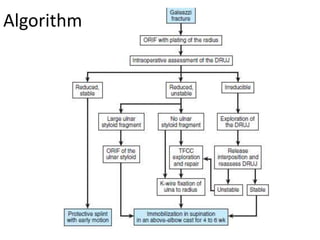
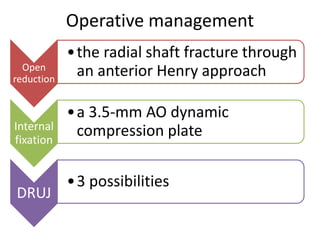
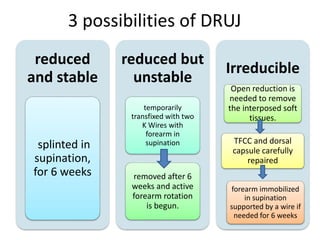
Galeazzi fracture-dislocation is a fracture of the distal or middle third of the radius shaft combined with dislocation of the distal radioulnar joint. It most often occurs in males due to indirect trauma from a fall on an outstretched hand with rotation. Radiographs show the radial fracture and dislocation of the distal radioulnar joint. Treatment involves open reduction and internal fixation of the radial fracture with a plate while restoring length and stability of the distal radioulnar joint. The forearm is then immobilized in supination for 4-6 weeks to heal.