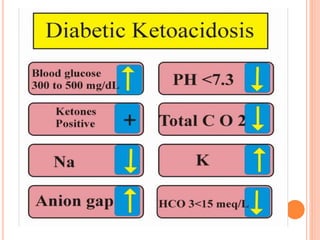
Diabetic ketoacidosis is a serious complication of diabetes that occurs when the body produces high levels of acids called ketones due to insufficient insulin. Signs include excessive thirst, frequent urination, nausea, abdominal pain, weakness, shortness of breath, and fruity breath. Treatment involves fluid and electrolyte replacement through IVs as well as insulin therapy to lower blood sugar and reverse the condition. Preventing DKA requires carefully managing diabetes through medication, monitoring blood sugar, adjusting insulin as needed, and seeking help when ill.