This document discusses fluid and electrolyte balance in newborns. Key points include:
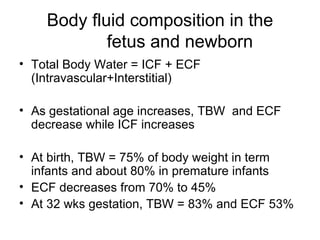
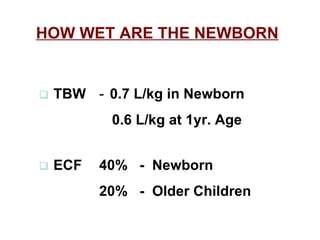
1) Total body water and extracellular fluid decrease as gestational age increases at birth, while intracellular fluid increases.
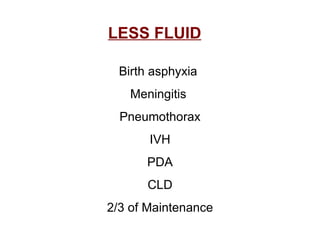
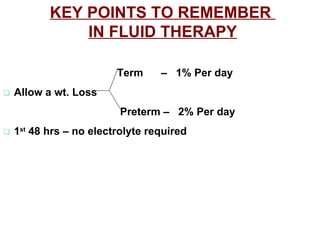
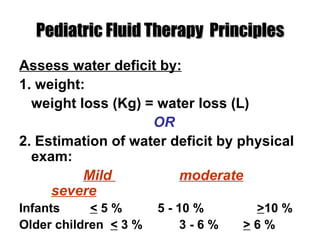
2) Term infants lose 5-10% of their body weight in the first few days of life due to reduction in extracellular fluid.
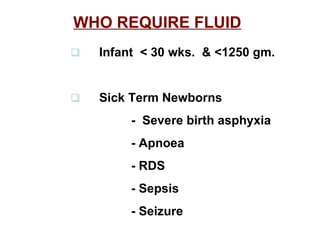
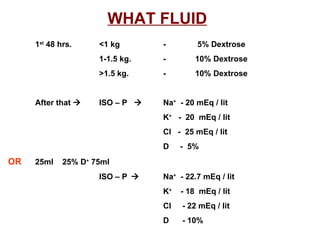
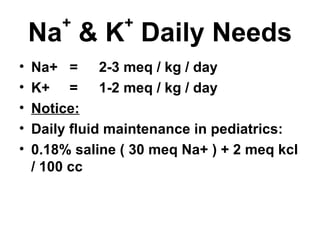
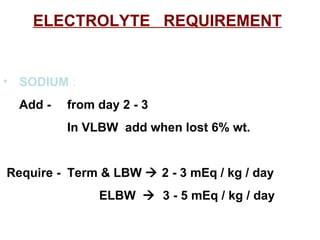
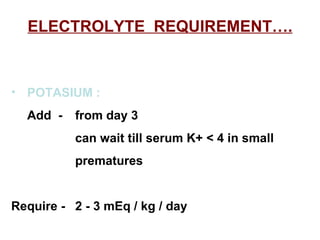
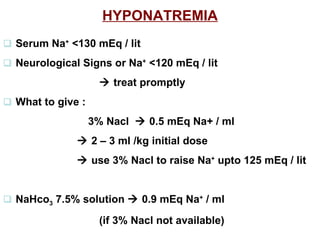
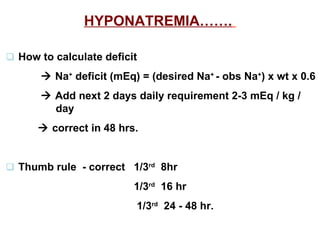
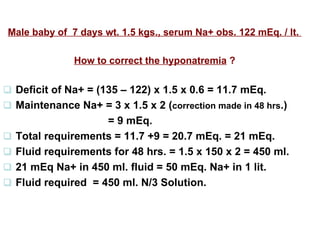
3) Preterm infants under 35 weeks gestation display negative sodium balance and hyponatremia in the first 2-3 weeks of life due to high renal sodium losses.
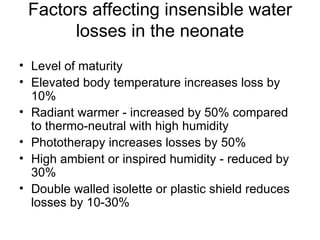
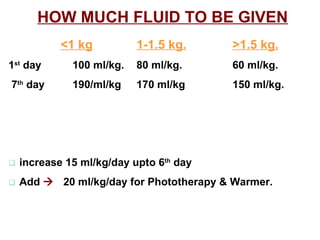
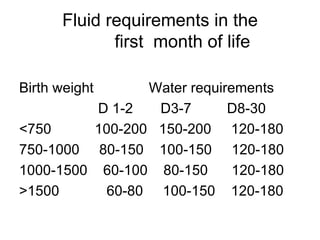
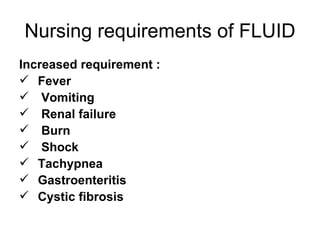
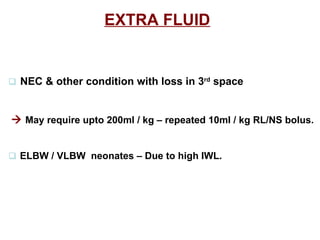
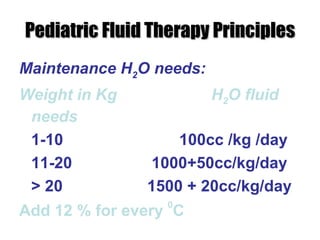
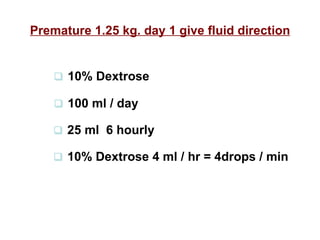
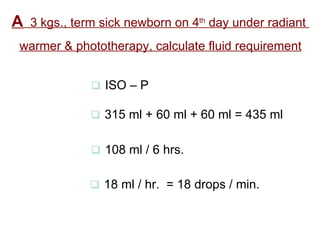
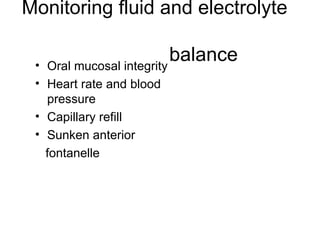
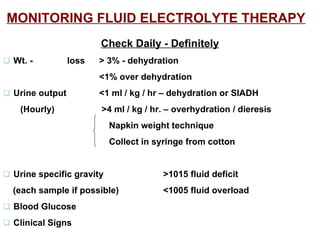
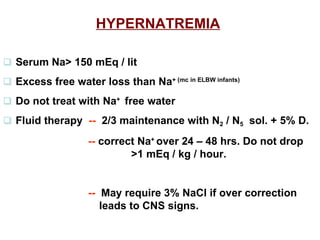
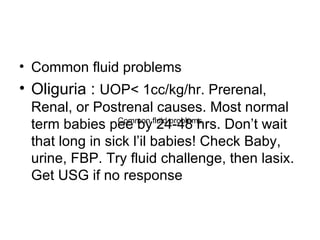
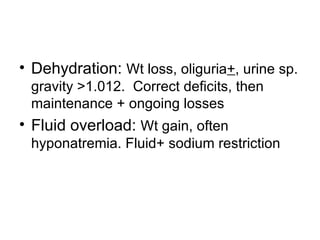
4) Fluid requirements vary based on weight, with very low birth weight infants needing higher amounts to offset insensible water losses. Close monitoring of fluid balance is important in