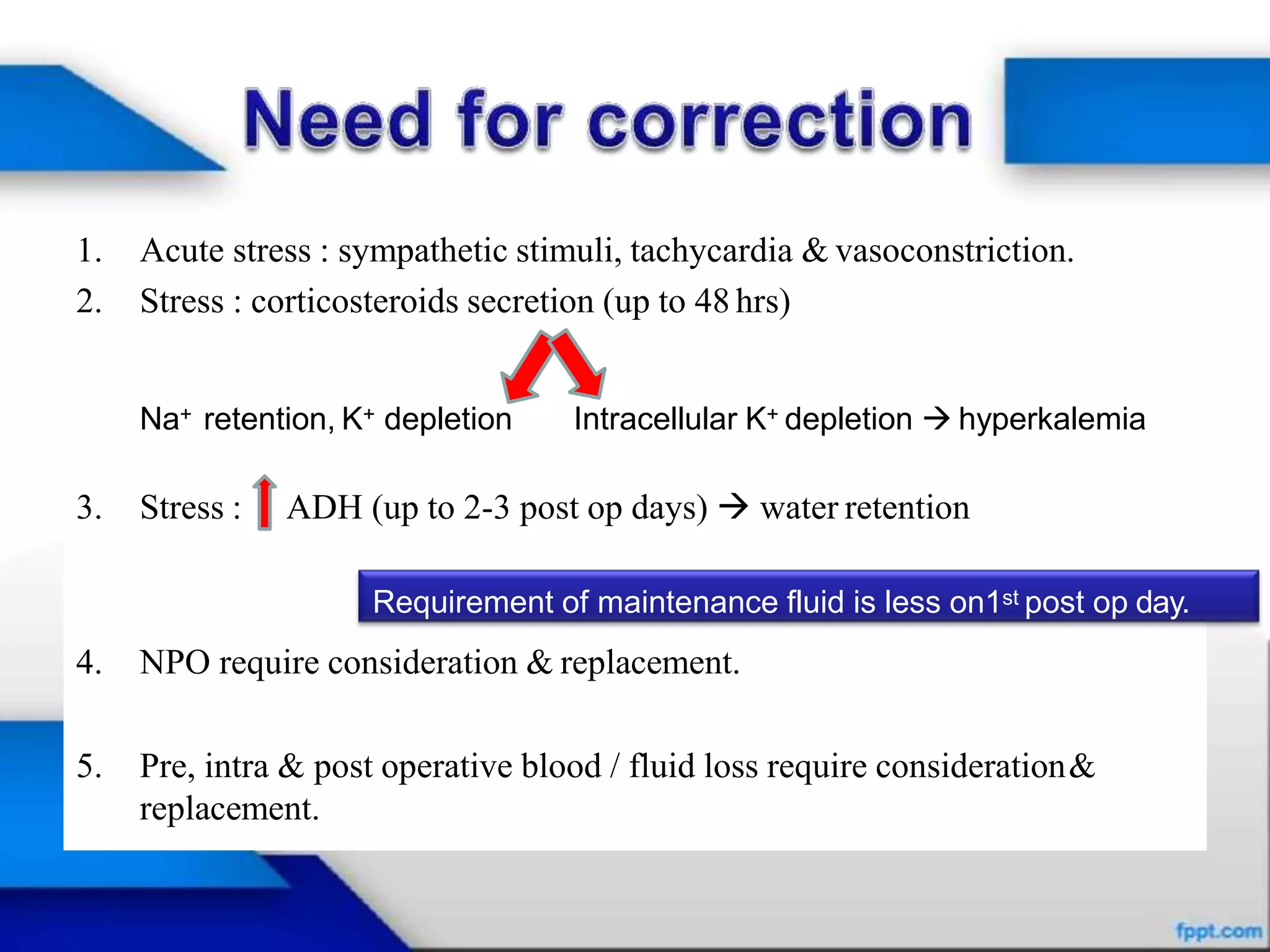
This document provides an overview of fluid therapy and electrolyte disturbances. It discusses the basic physiology of body fluids, including total body water content and distribution. It then covers various electrolyte abnormalities like hyponatremia, hypernatremia, hypokalemia, hyperkalemia, hypocalcemia, hypercalcemia, hypomagnesemia, and hypermagnesemia. It also addresses acid-base balance disturbances and different intravenous fluid options for fluid resuscitation and maintenance.