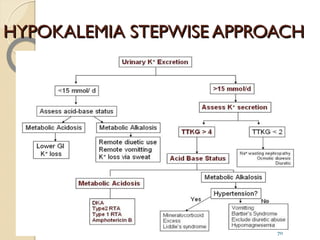
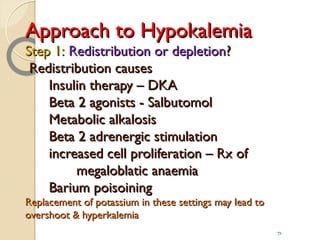
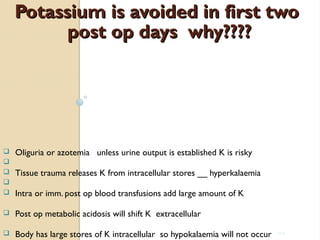
Here are the key steps in approaching hypokalemia:
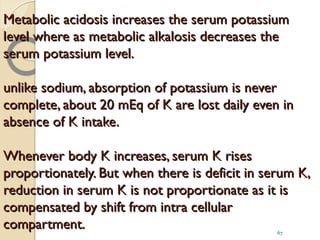
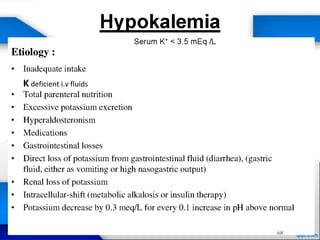
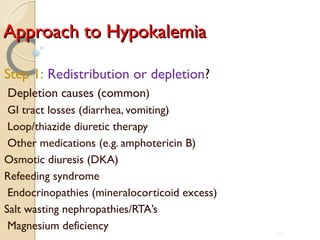
1. Determine if the hypokalemia is caused by redistribution or depletion. Redistribution occurs with insulin, beta-agonists, alkalosis etc. and replacement may cause overshoot hyperkalemia. Depletion is more common, due to GI losses, diuretics, medications etc.
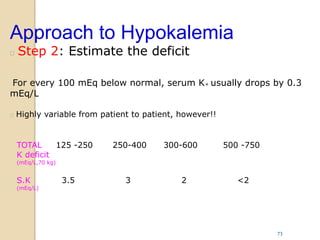
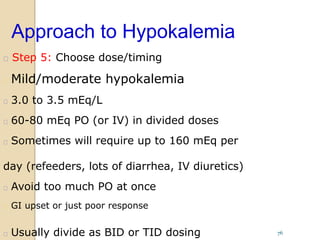
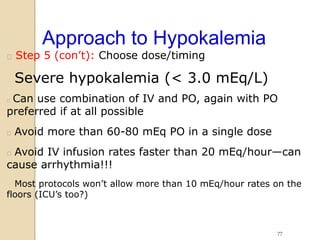
2. Estimate the potassium deficit based on how low the serum potassium is. A deficit of 100-250 mEq is suggested for levels of 3.5-3 mEq/L.
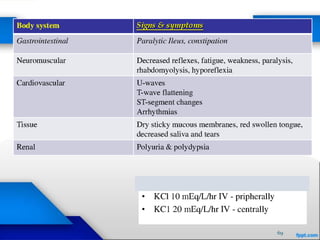
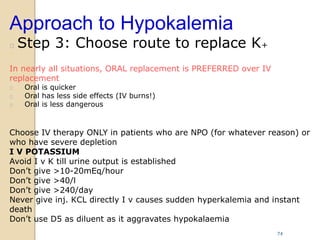
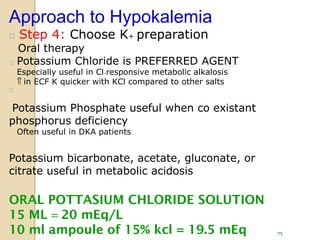
3. Choose oral replacement whenever possible over IV, as oral is safer and better tolerated. Only use IV if patient cannot take oral or deficit is severe.
4