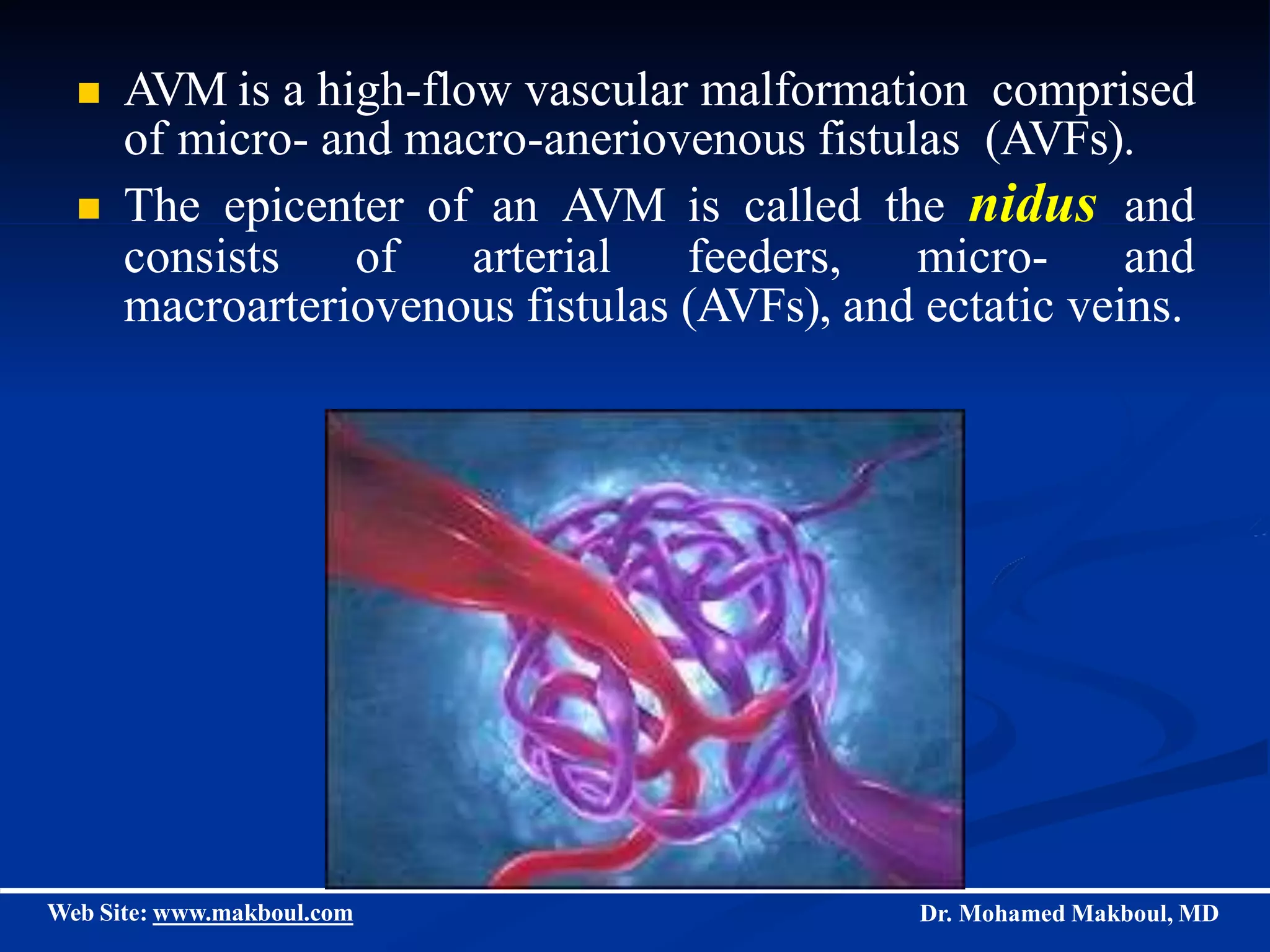
Haemangiomas and vascular malformations can be classified into two groups: haemangiomas and vascular malformations. Haemangiomas are common tumors in infancy that exhibit rapid growth and slow regression during childhood. Vascular malformations are present at birth and never regress, comprised of abnormally formed blood vessels. Common types of vascular malformations include slow-flow malformations (capillary, lymphatic, venous) and fast-flow malformations (arterial, arteriovenous fistulae, arteriovenous malformations). Diagnostic imaging and clinical presentation can help distinguish between haemangiomas and vascular malformations and their subtypes. Treatment depends on the specific diagnosis and may include observation, medications, laser therapy,