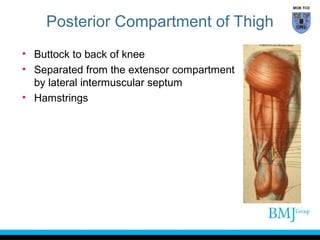
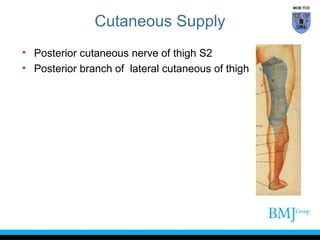
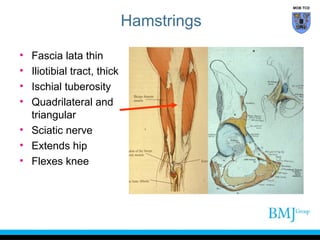
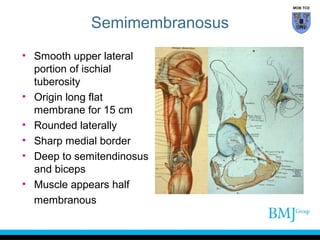
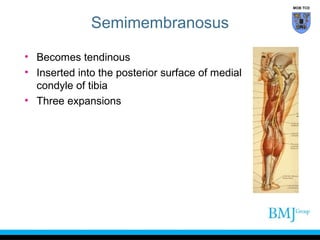
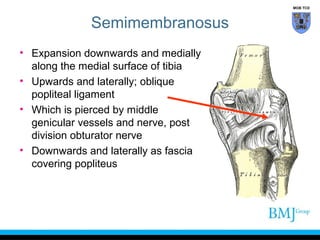
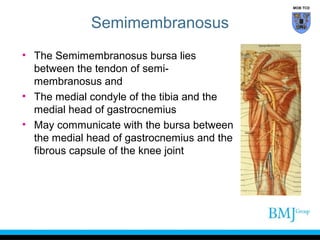
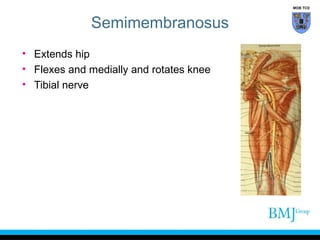
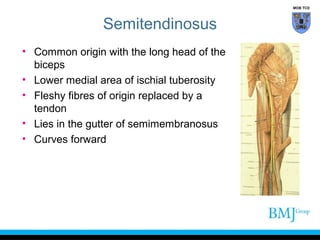
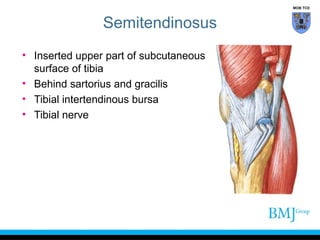
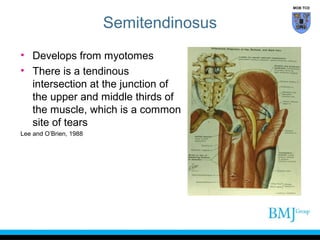
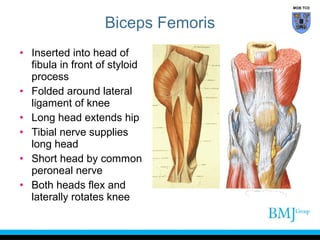
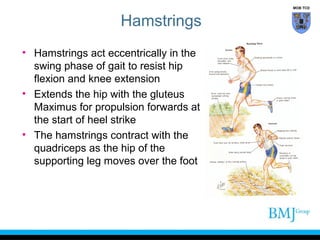
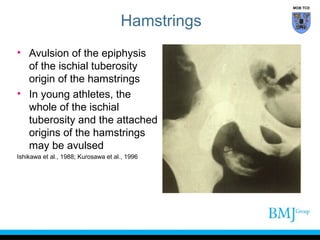
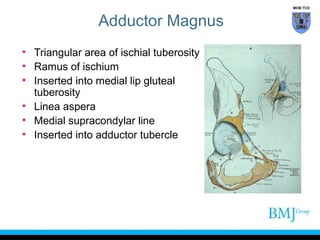
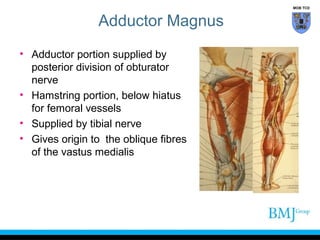
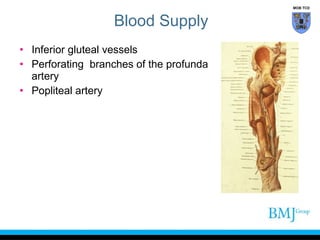
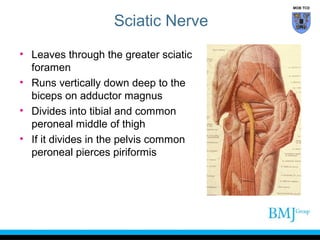
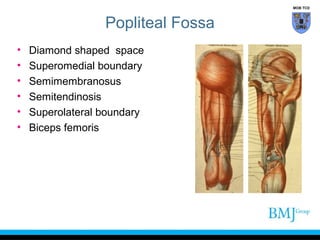
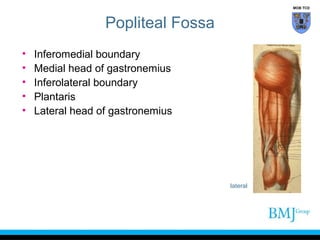
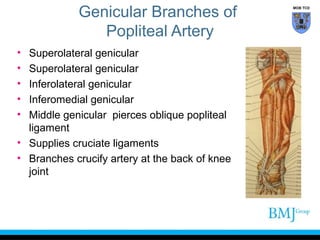
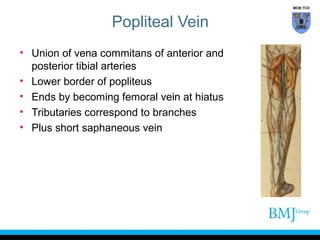
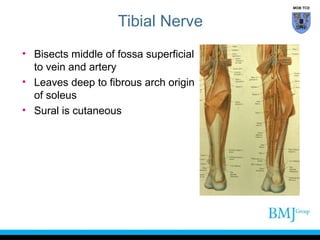
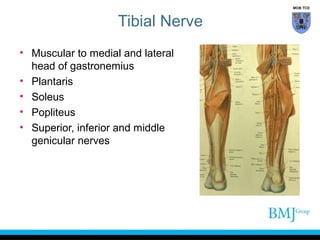
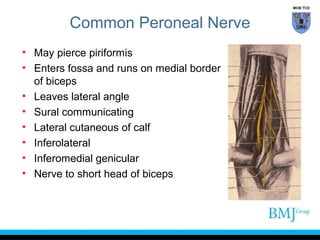
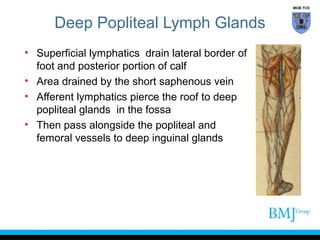
This document provides information on the posterior compartment of the thigh. It describes the anatomy of the hamstring muscles - semimembranosus, semitendinosus, and biceps femoris - including their origins, insertions, innervation and actions. It also discusses the popliteal fossa and its contents, including the popliteal artery and veins, tibial and common peroneal nerves, and lymph nodes. Injuries to the hamstrings and neurovascular structures in the popliteal fossa are mentioned.