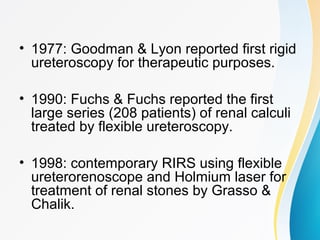
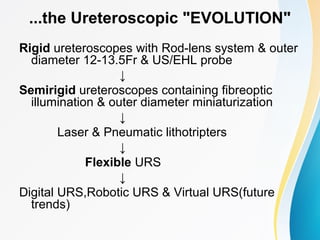
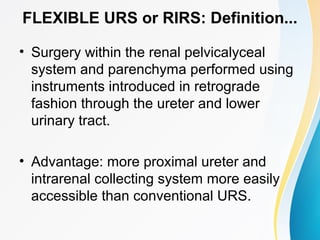
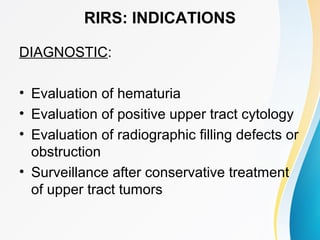
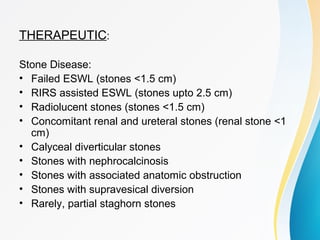
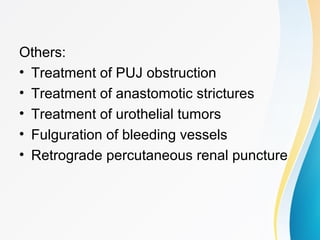
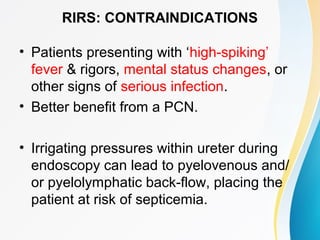
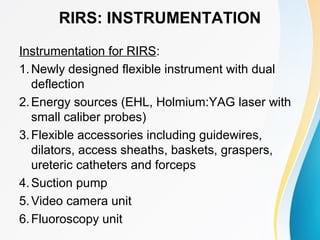
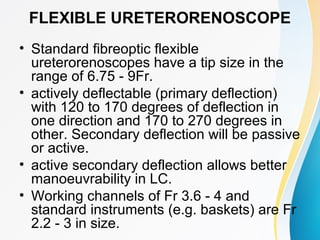
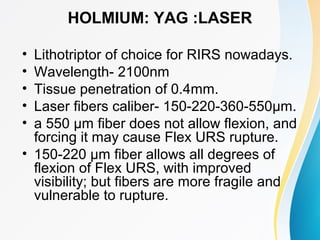
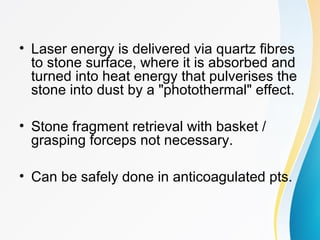
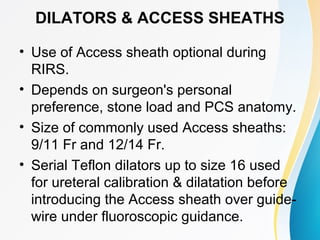
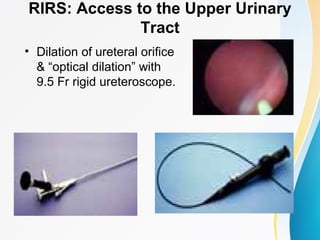
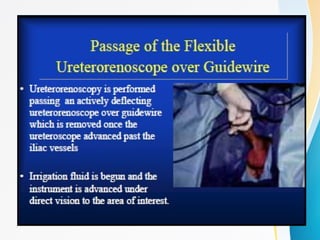
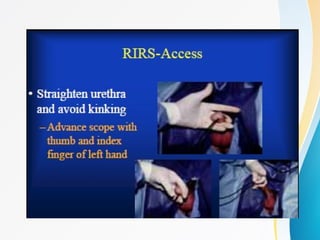
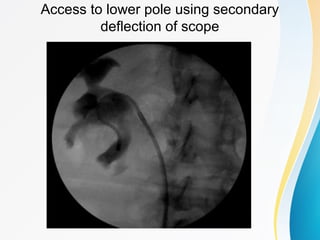
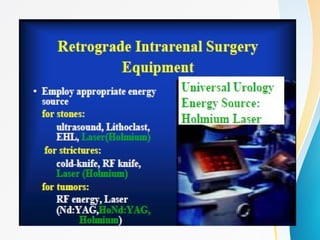
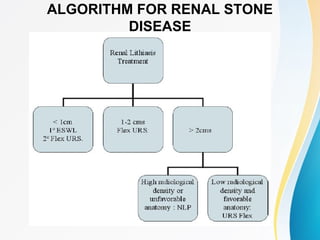
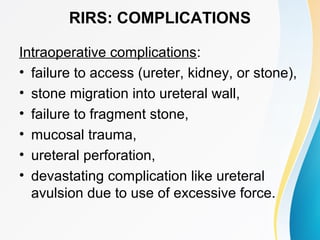
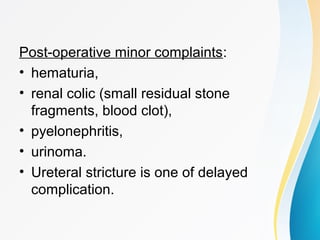
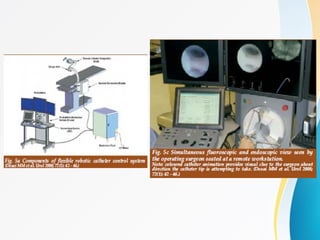
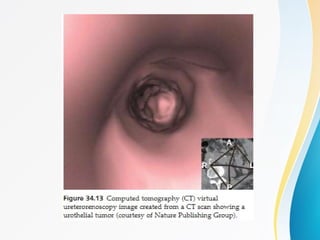
This document discusses flexible ureterorenoscopy (RIRS) for treating conditions of the kidney and urinary tract. RIRS uses flexible instruments introduced through the ureter to access the kidney in a minimally invasive manner. It has advantages over rigid ureteroscopy like shorter hospital stays and recovery time. The document outlines the history, indications, instrumentation, technique and complications of RIRS. Emerging technologies discussed include digital flexible ureteroscopy, flexible robotic assistance and virtual reconstruction of ureteroscopic views.