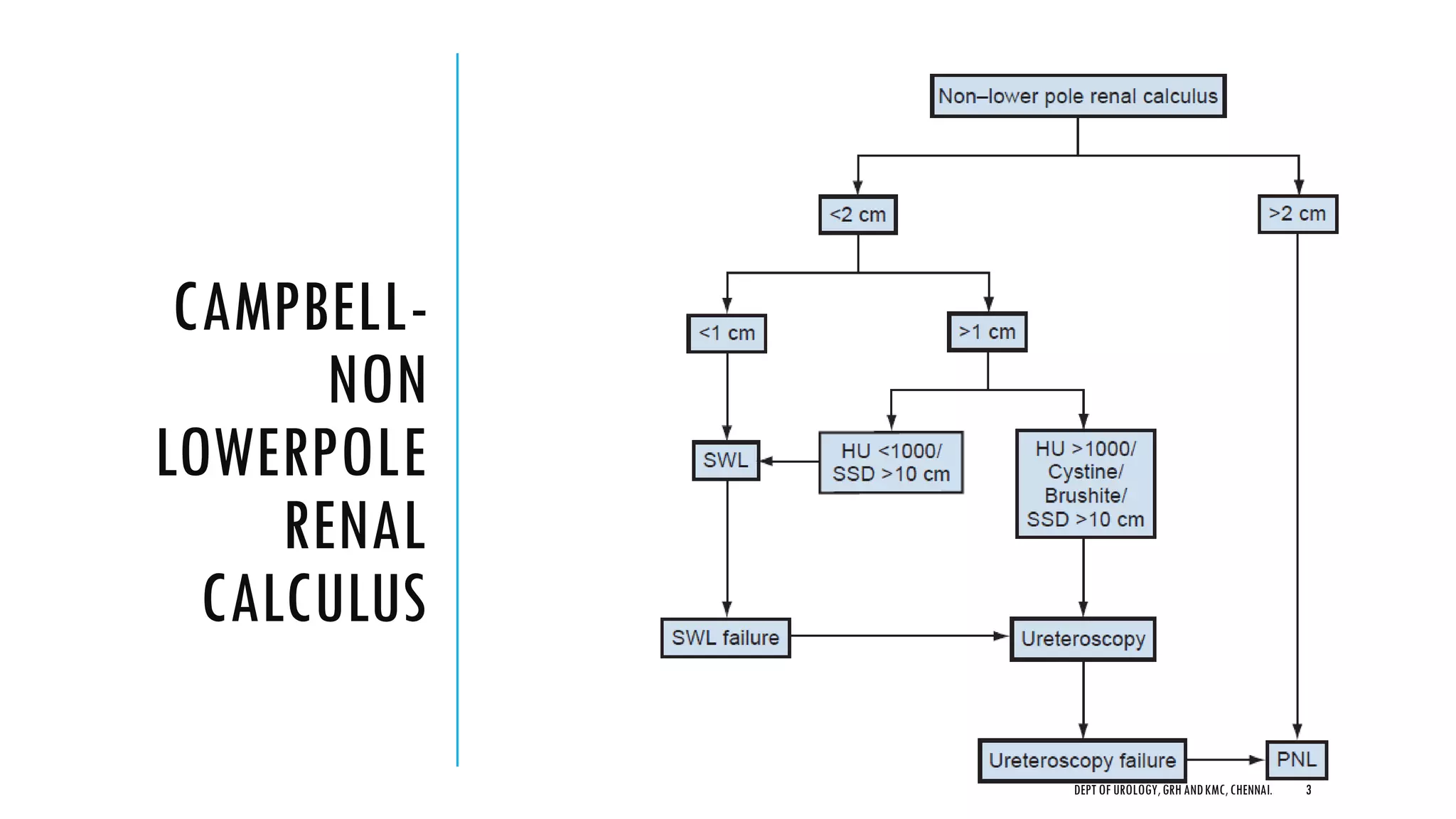
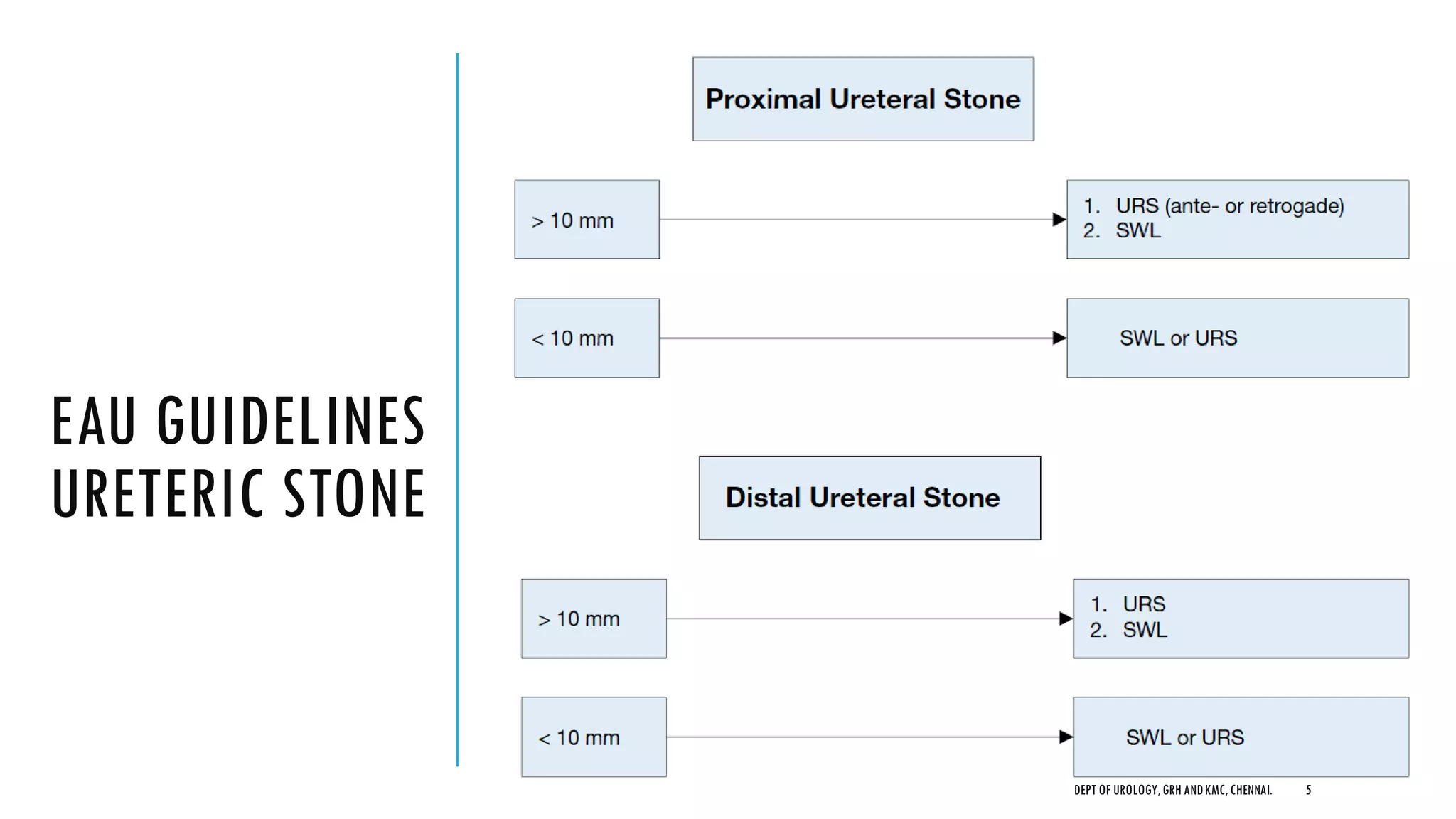
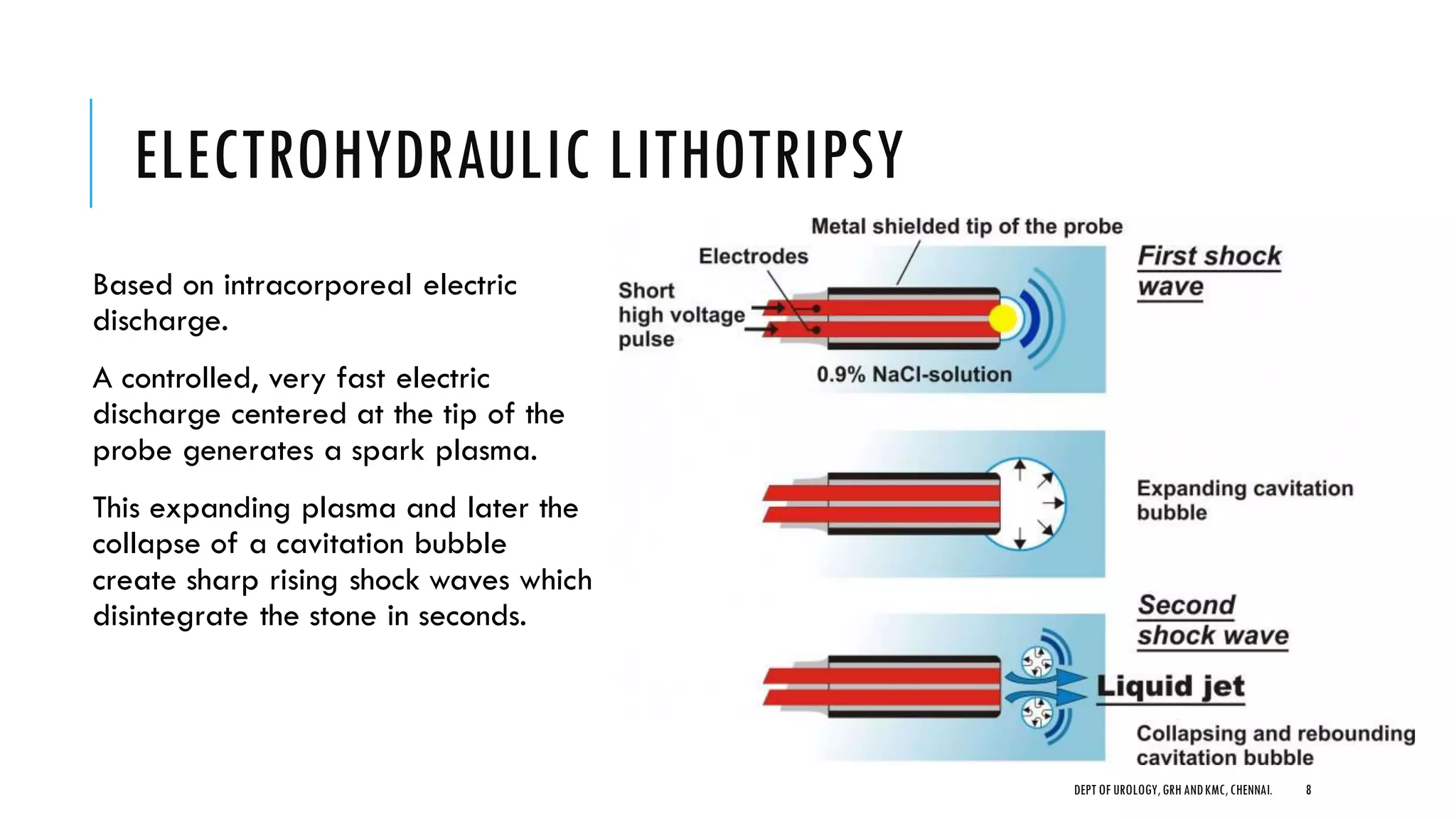
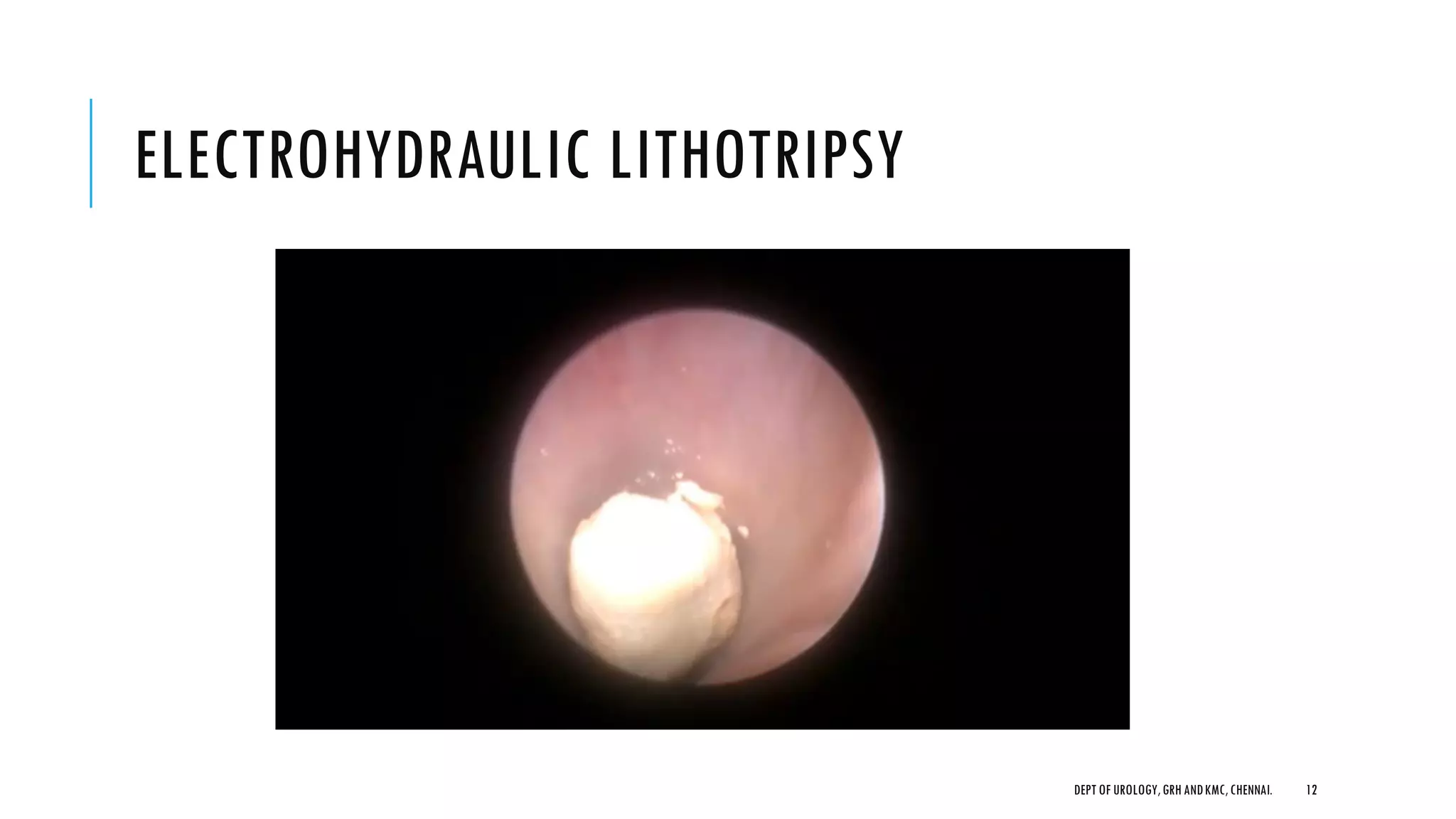
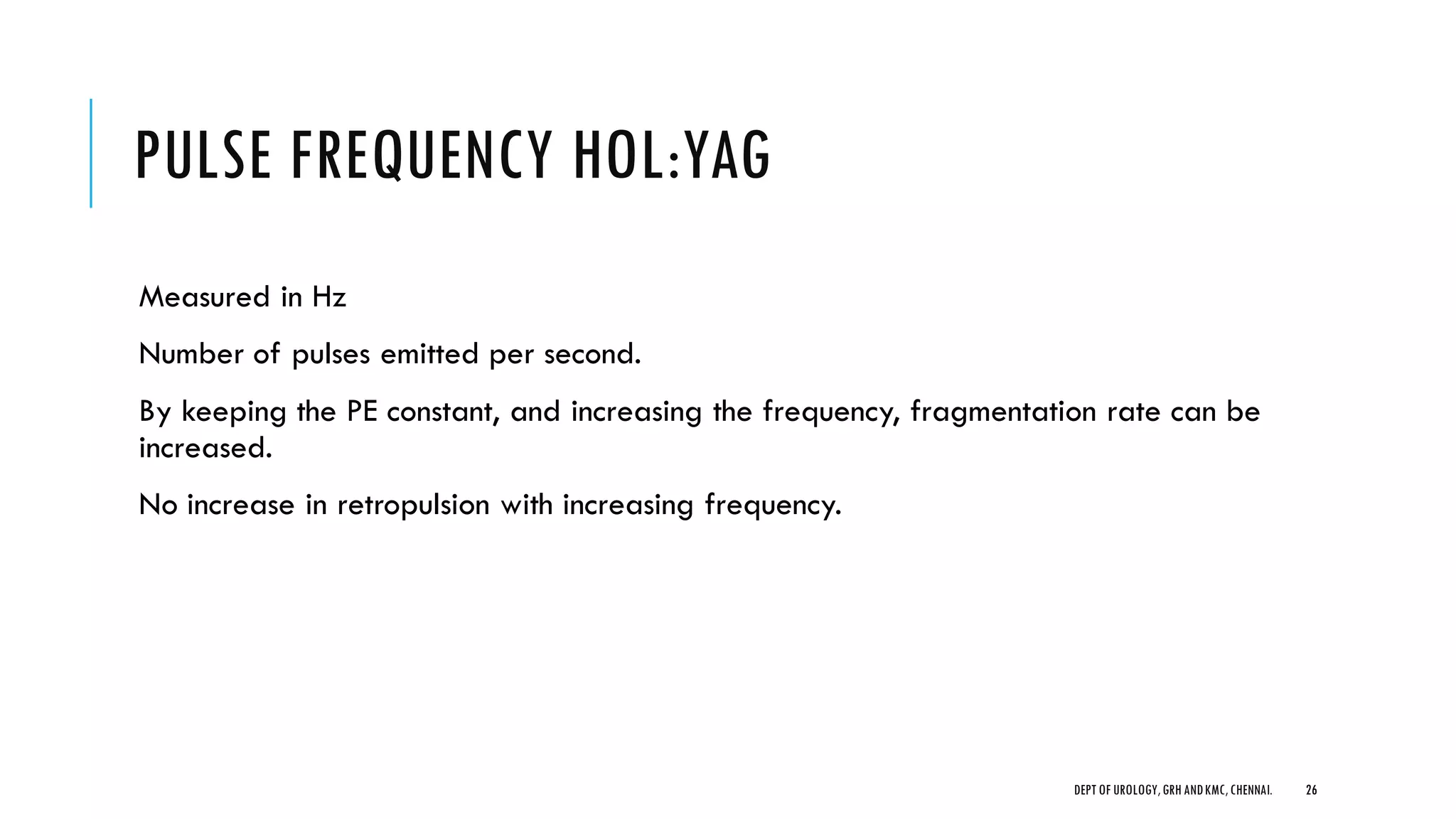
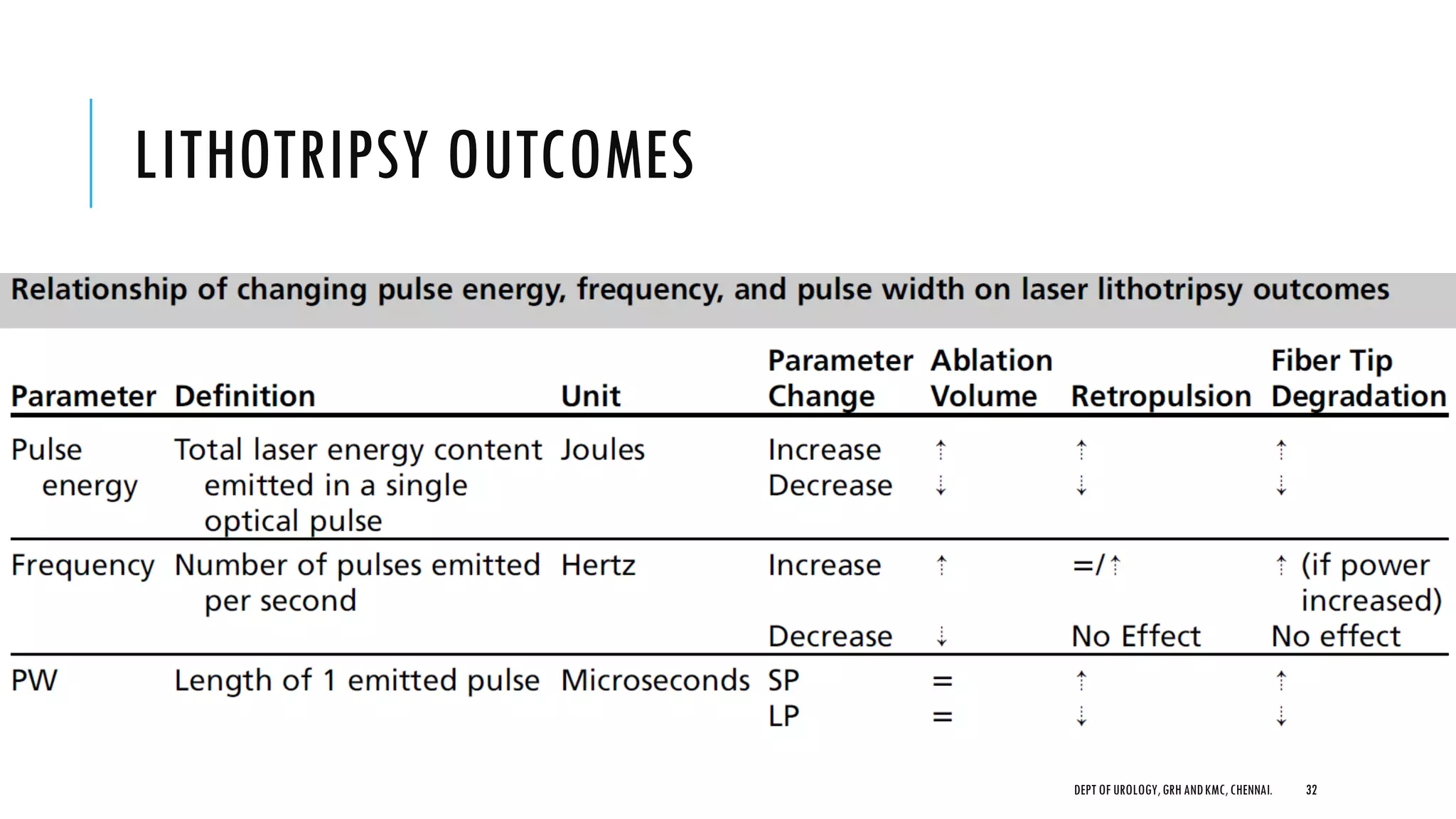
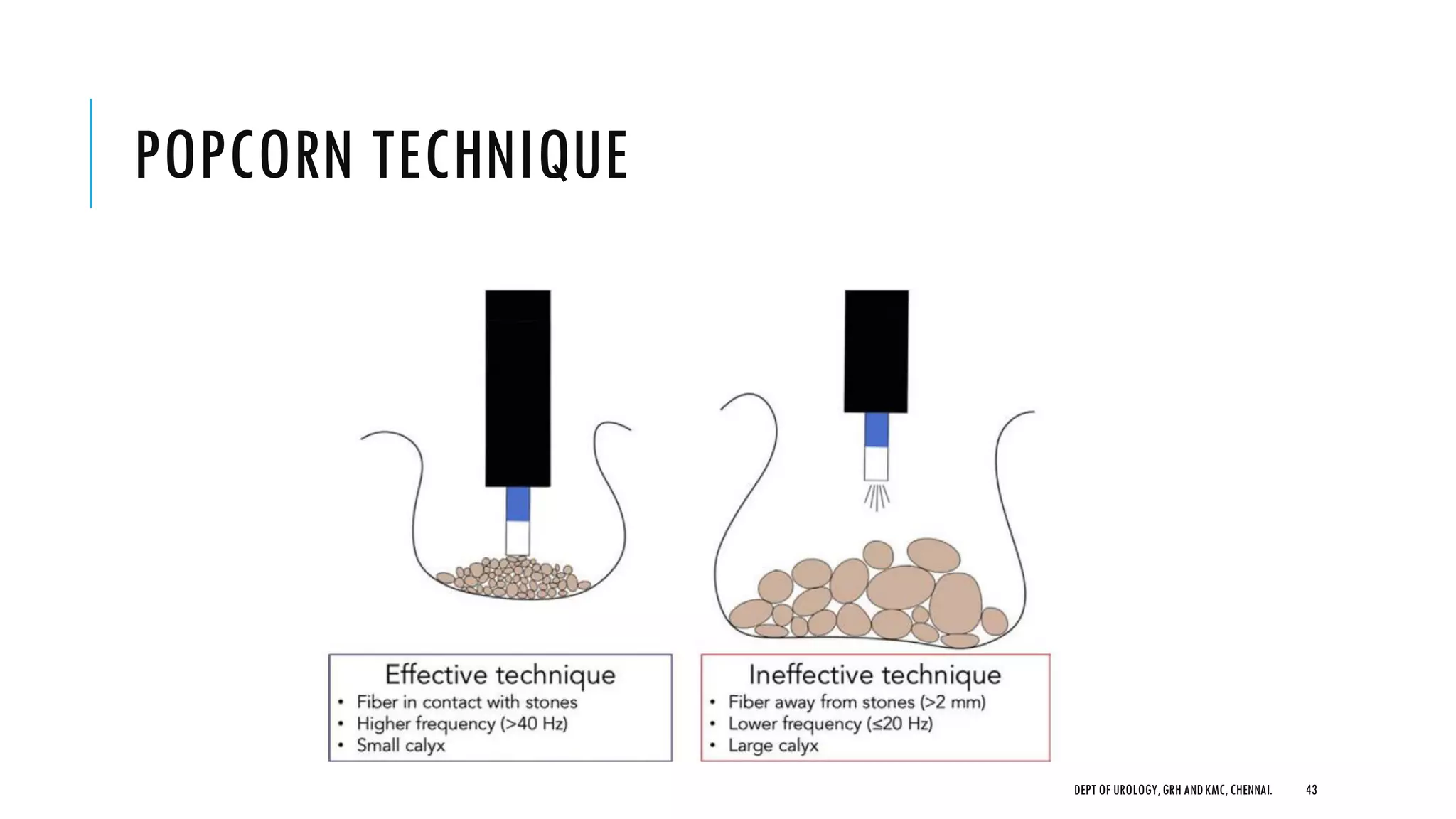
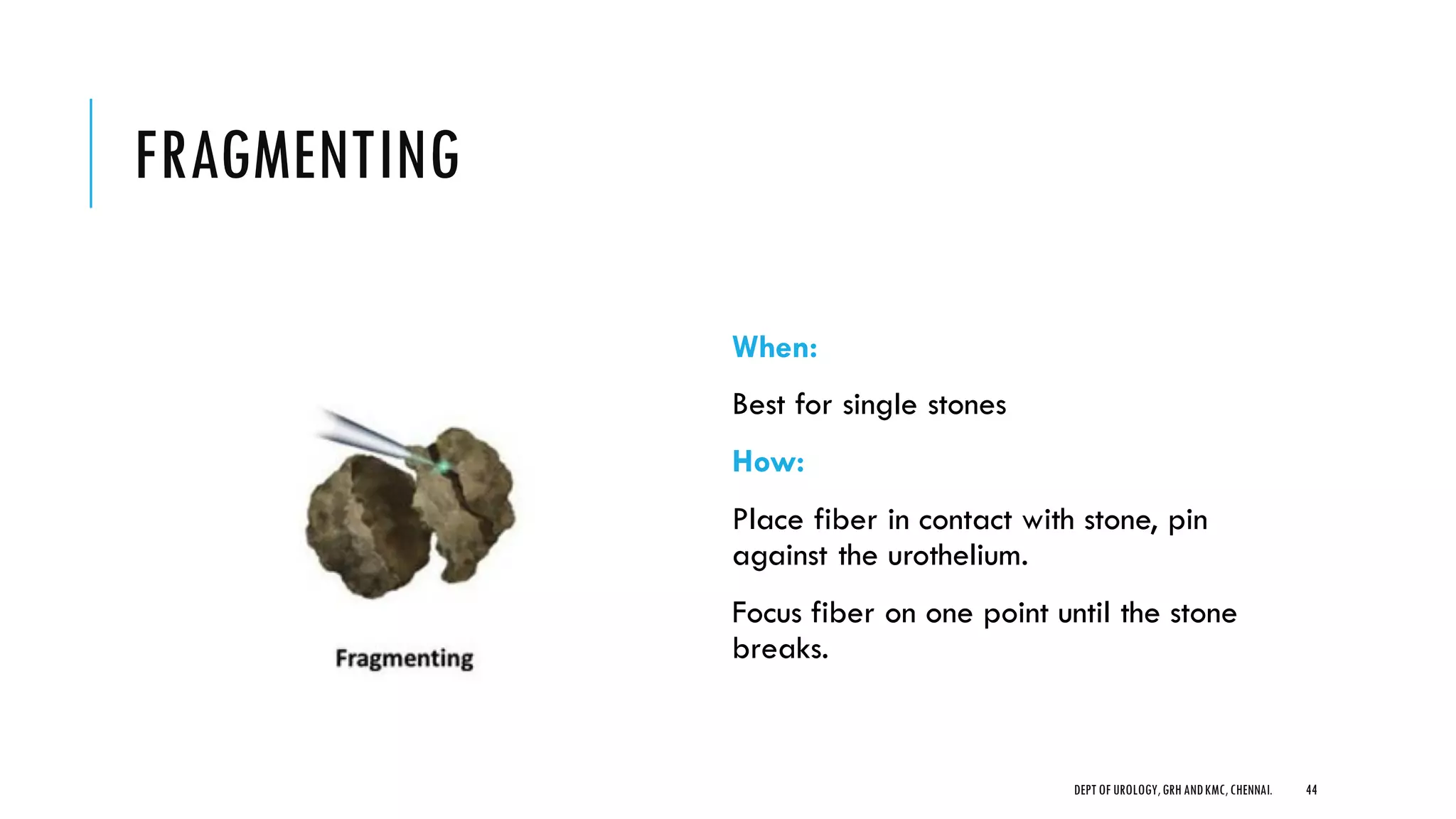
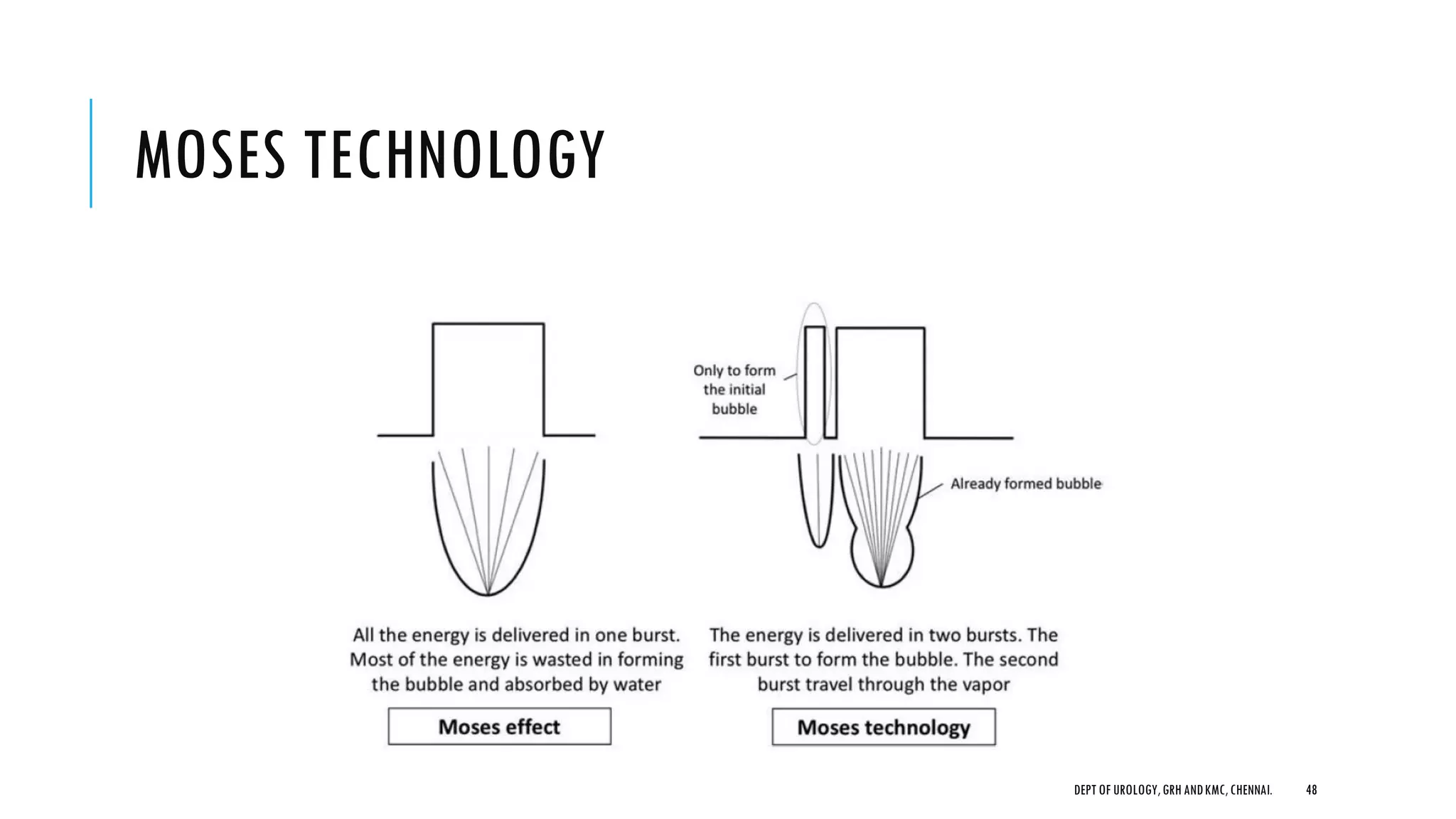
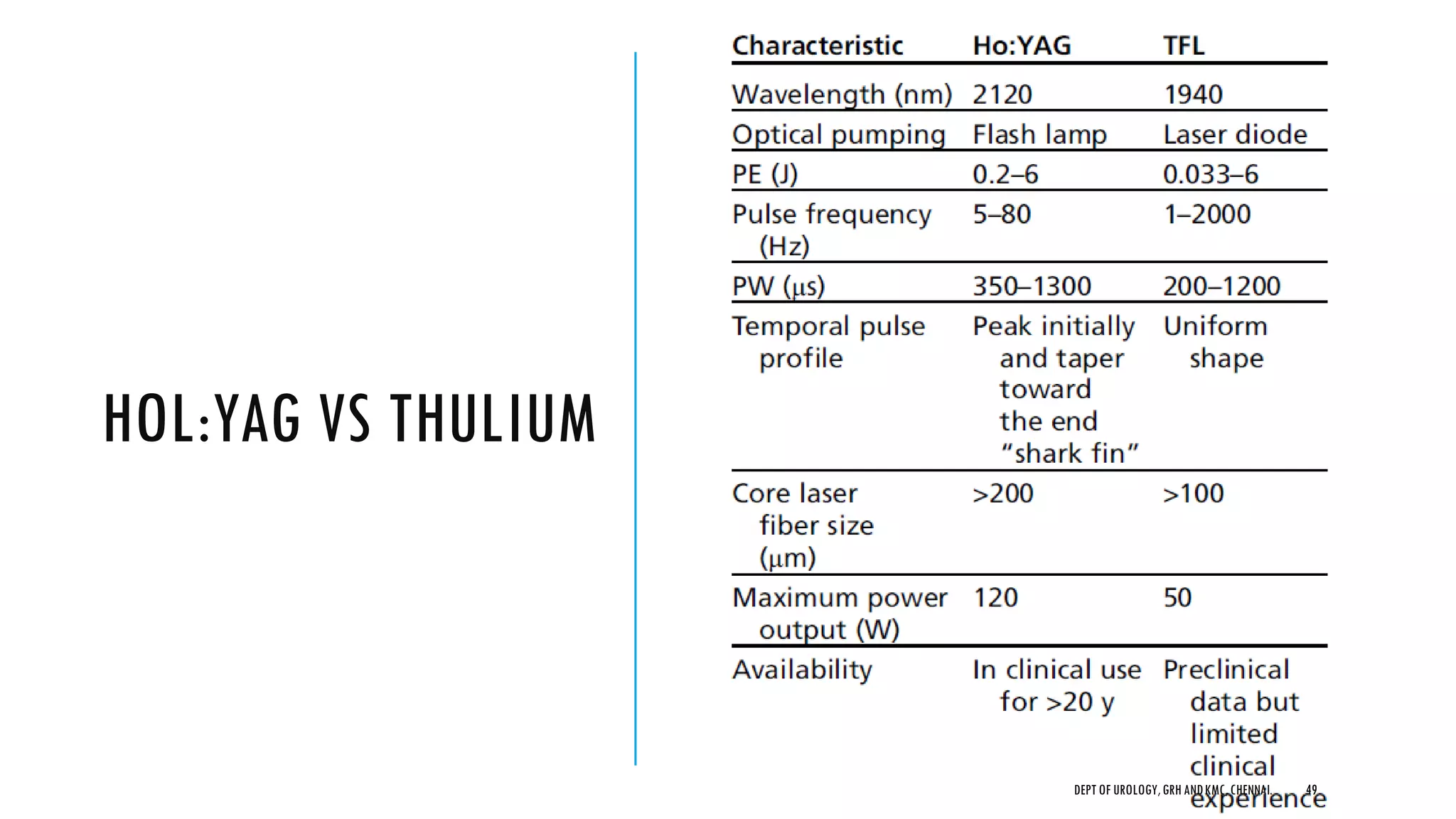
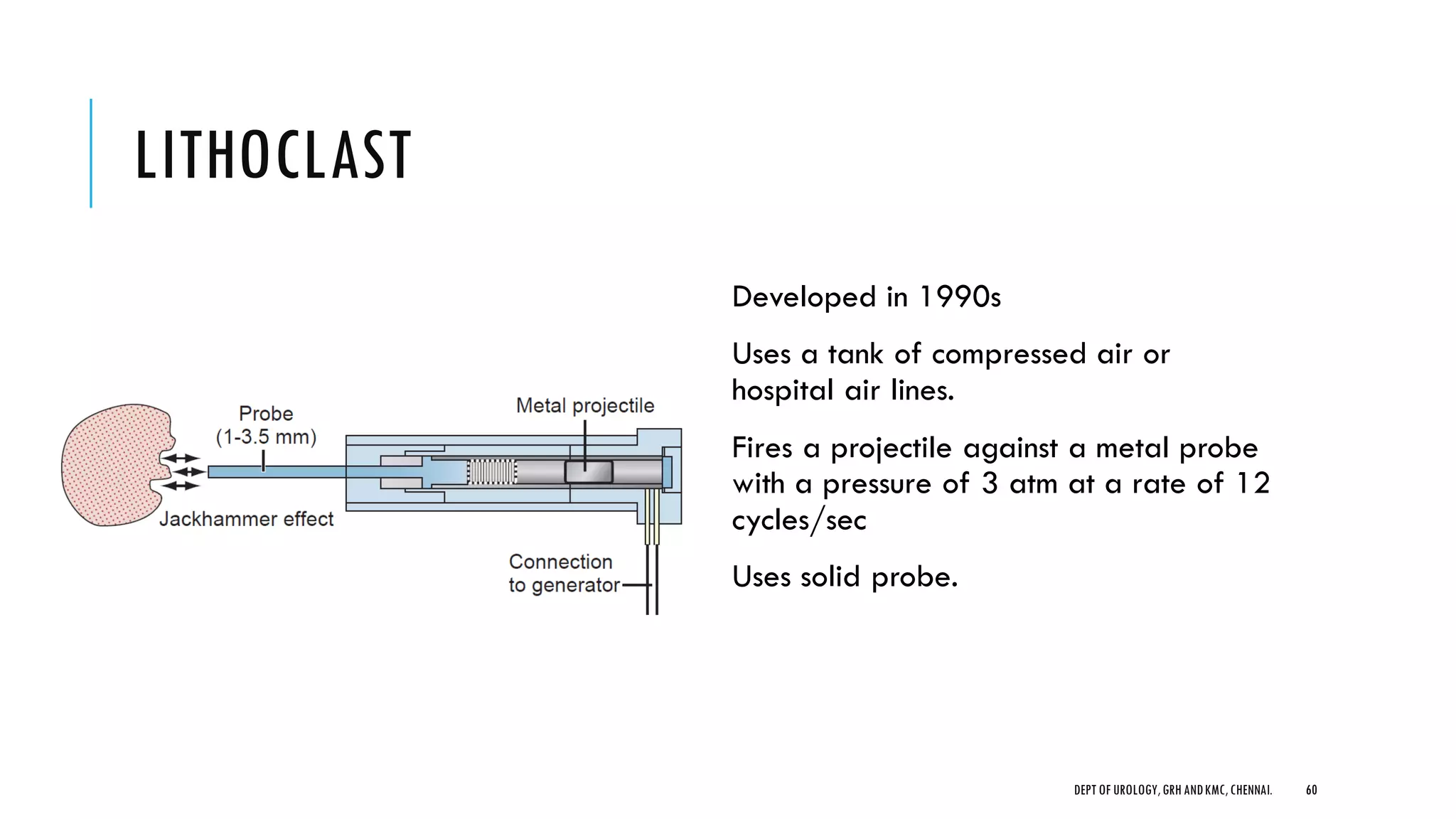
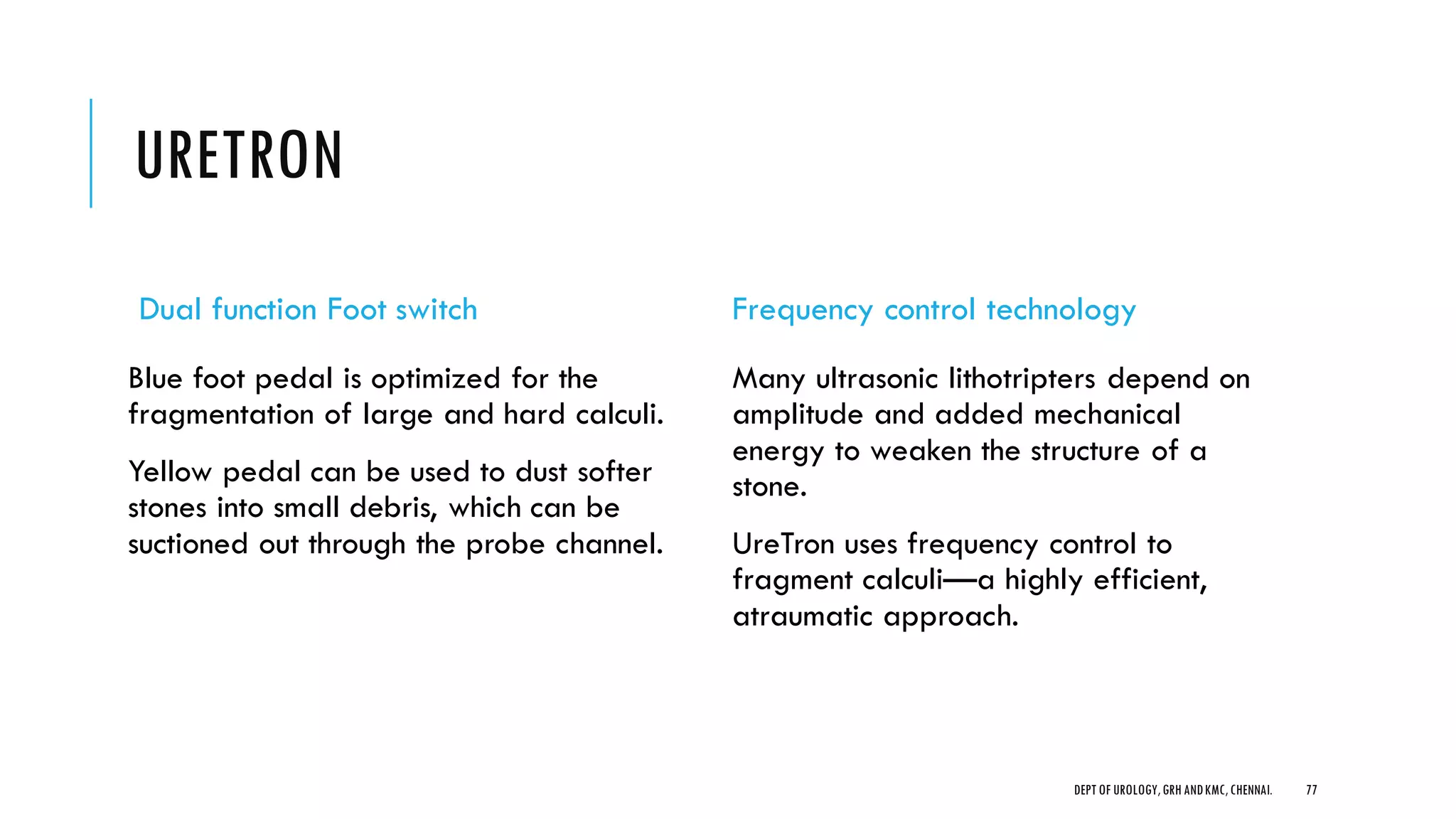
This document summarizes information about various techniques for intracorporeal lithotripsy presented by the Department of Urology at GRH and KMC in Chennai. It discusses the principles and techniques of electrohydraulic lithotripsy, laser lithotripsy using holmium:YAG lasers, and ballistic lithotripsy. Details are provided on the components of laser fibers, different laser settings and techniques for stone fragmentation, and devices used for preventing stone retropulsion. A variety of lithotripters employing different energy sources for ballistic lithotripsy are also summarized.