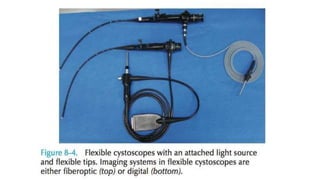
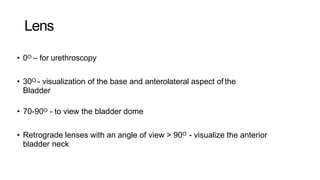
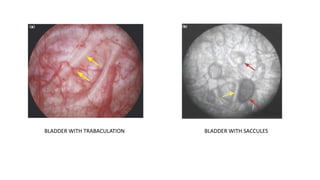
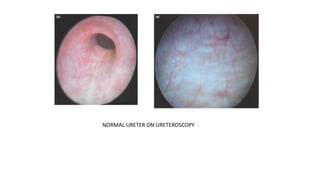
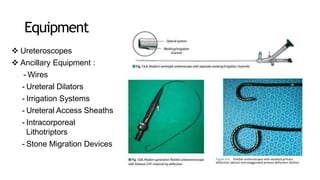
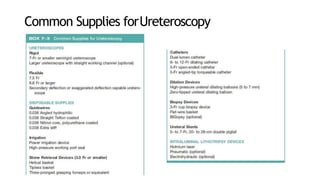
The document details various types of endourology procedures, including cystourethroscopy and ureteroscopy, which are used for diagnostic and therapeutic interventions in the urinary tract. It outlines the advantages and techniques of rigid and flexible cystoscopes, as well as the necessary patient preparation and techniques for ureteroscopy. Key components and equipment needed for these procedures are also highlighted, emphasizing considerations for safety and effectiveness.