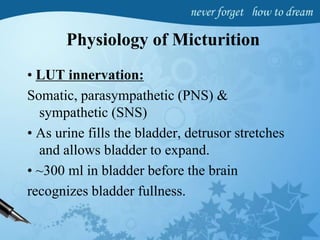
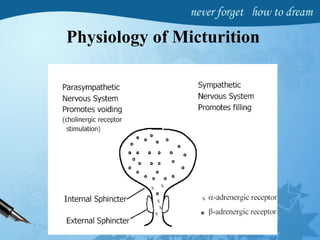
This document provides an overview of urodynamics, including the physiology of micturition, urodynamics equipment, cystometry, uroflowmetry, pressure flow studies, and abnormal findings. Key points include:
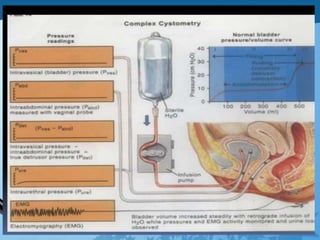
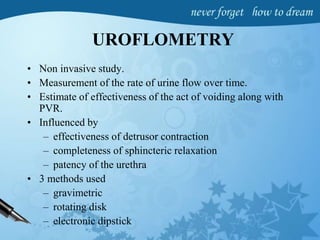
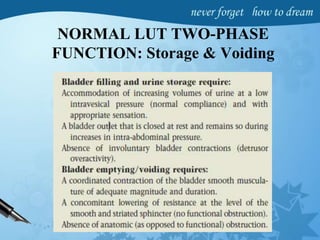
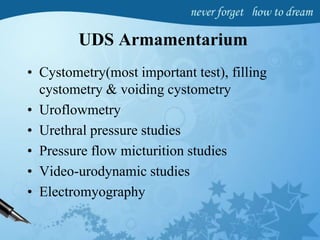
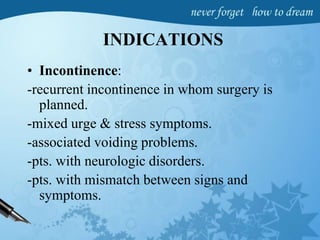
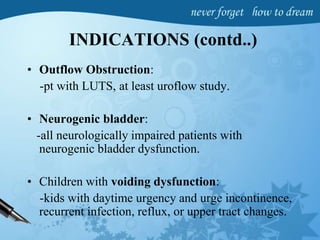
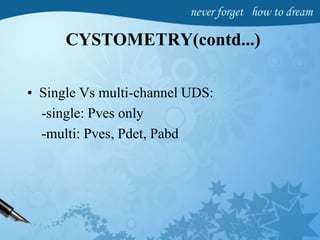
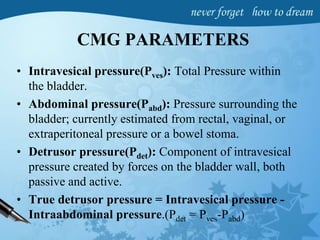
1. Urodynamics evaluates bladder filling, storage, and emptying through tests like cystometry, uroflowmetry, and pressure flow studies.
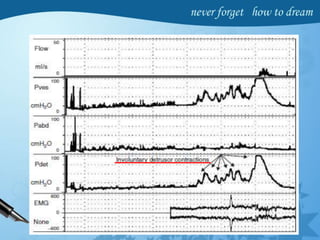
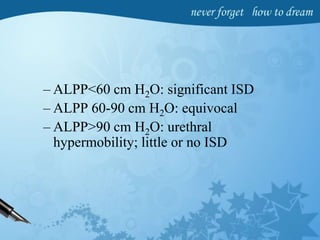
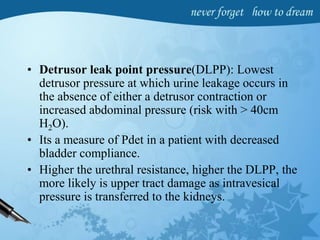
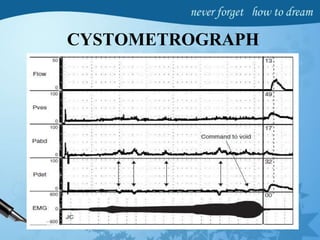
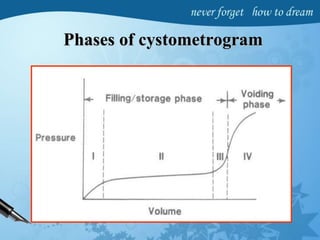
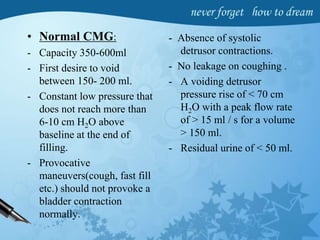
2. Cystometry measures bladder pressure during filling and identifies abnormalities like impaired compliance, detrusor overactivity, and high leak point pressures.
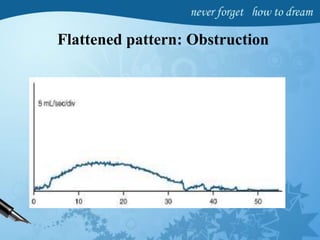
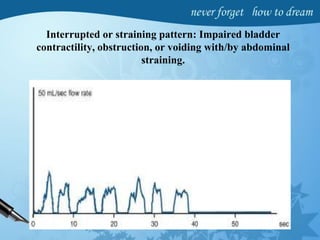
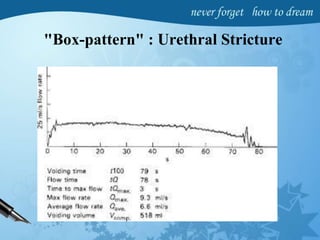
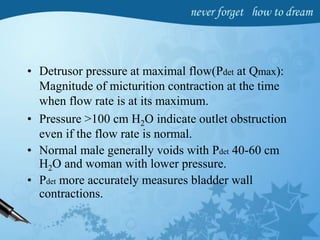
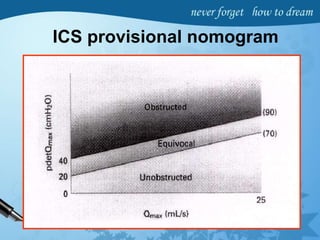
3. Pressure flow studies quantify voiding and help differentiate obstruction from poor contractility.
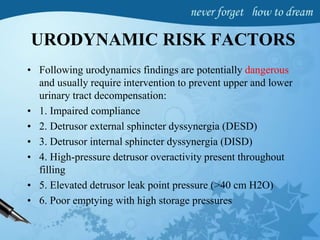
4. Abnormal findings on urodynamics like high pressures, impaired compliance,
![Impaired compliance is seen in:
• neurologic conditions: spinal cord injury/lesion,
spina bifida, usually results from increased outlet
resistance (e.g., detrusor external sphincter
dyssynergia [DESD]) or decentralization in the
case of lower motor neuron lesions,
• Long-term BOO (e.g., from benign prostatic
obstruction),
• Structural changes- radiation cystitis or
tuberculosis.
• Impaired compliance with prolonged elevated
storage pressures is a urodynamic risk factor and
needs treatment to prevent renal damage.](https://image.slidesharecdn.com/uds-160825114502/85/Urodynamic-studies-24-320.jpg)