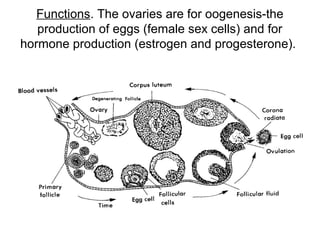
This document defines key terms related to female reproductive anatomy and physiology. It describes the internal reproductive organs including the uterus, fallopian tubes, ovaries, and vagina. It discusses their locations, structures, and main functions. It also explains the female menstrual cycle and hormone production, the process of egg production and development within the ovaries, and the external female reproductive organs.