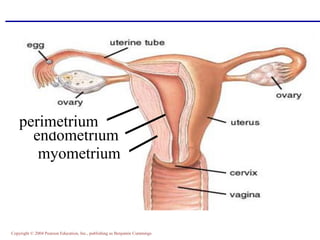
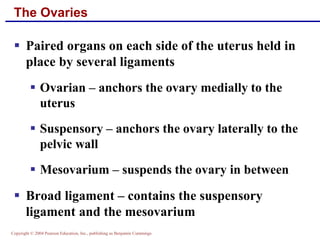
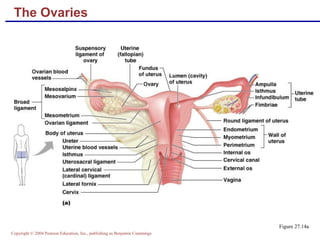
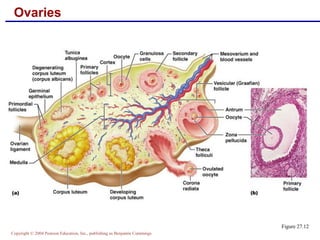
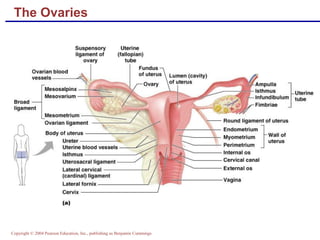
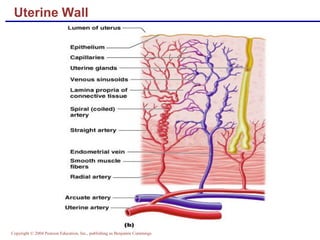
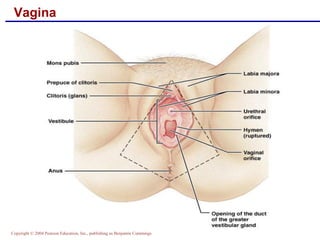
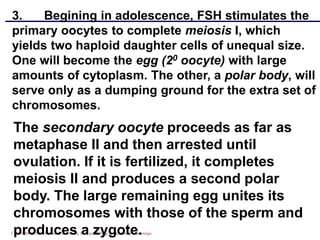
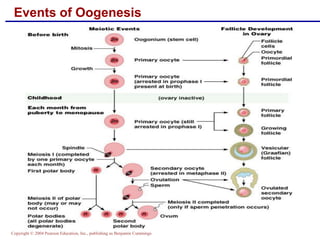
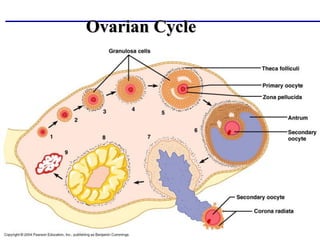
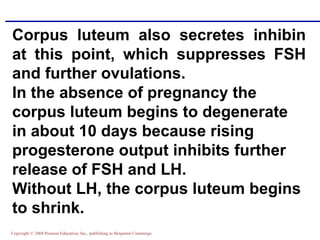
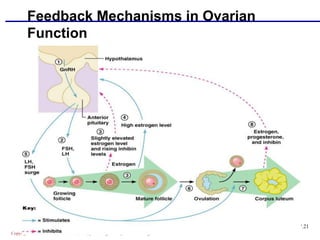
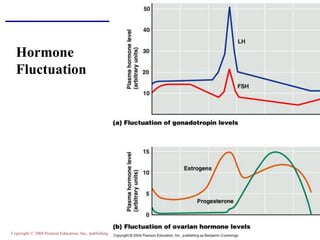
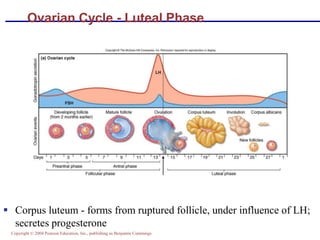
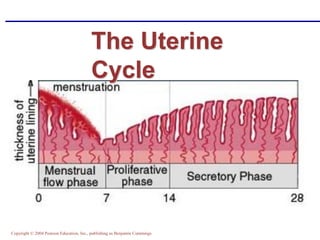
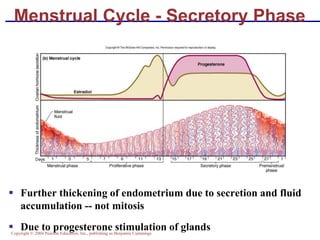
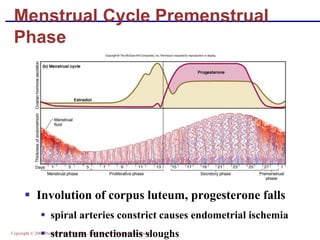
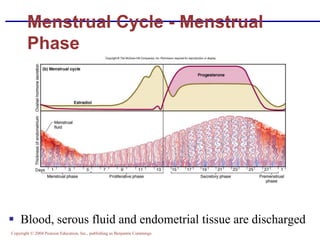
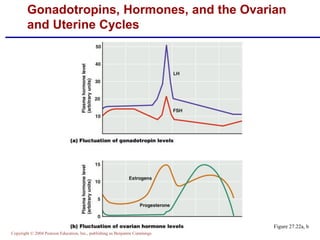
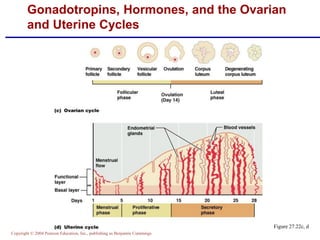
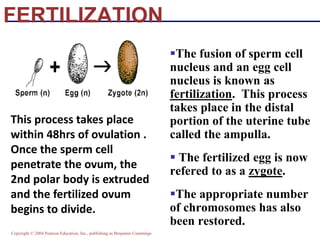
The document summarizes the key components of the female reproductive system, including both internal and external structures. The internal structures include the ovaries, fallopian tubes, uterus, cervix, and vagina. The ovaries contain follicles that contain oocytes and produce hormones. During ovulation, a mature follicle ruptures and releases an oocyte. If fertilized by sperm in the fallopian tubes, the fertilized egg implants in the uterus which nourishes the developing embryo. The menstrual cycle is regulated by changes in the ovaries and uterus across the follicular, ovulation, and luteal phases.