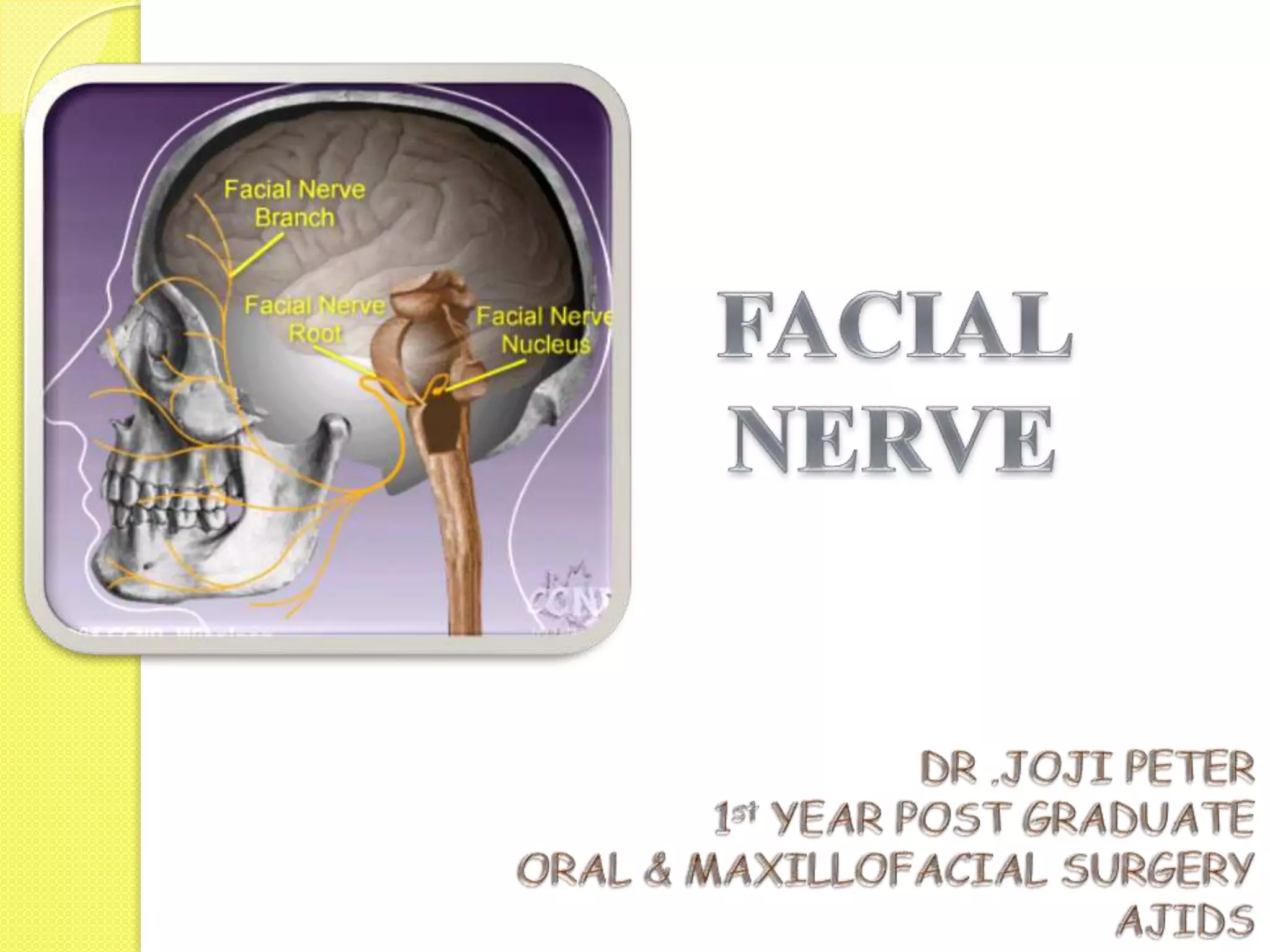
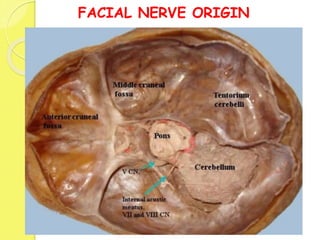
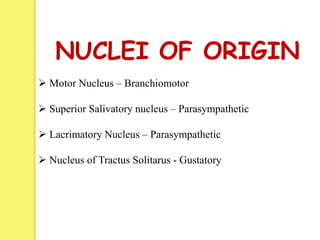
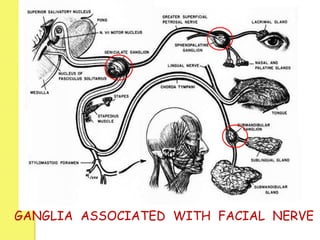
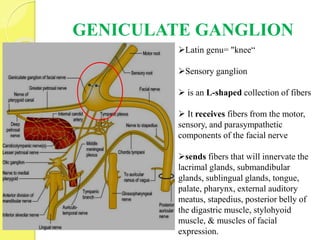
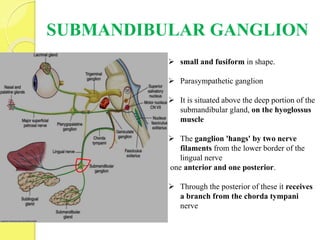
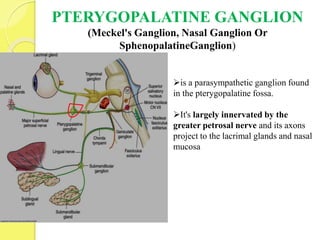
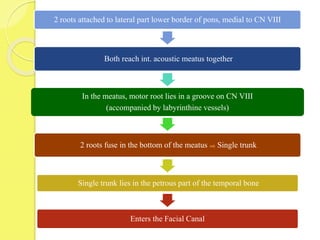
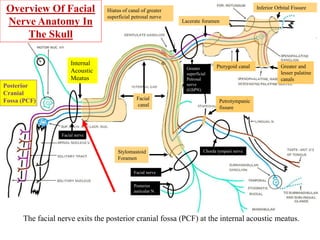
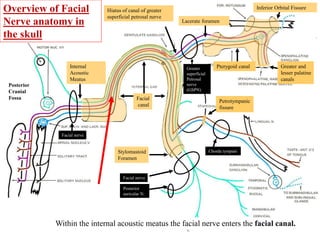
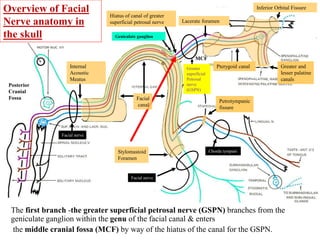
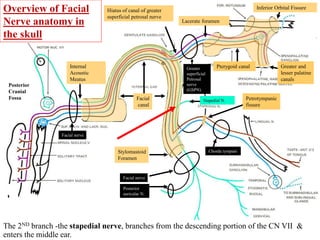
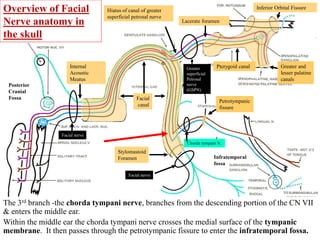
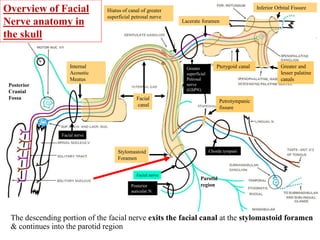
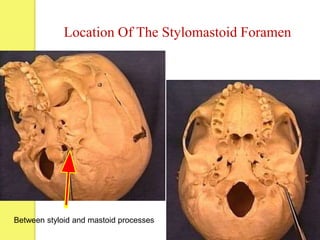
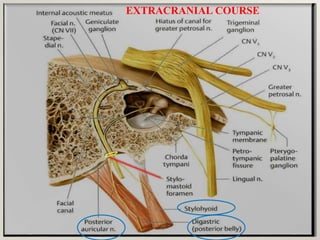
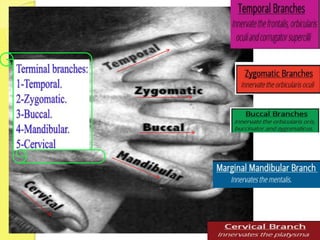
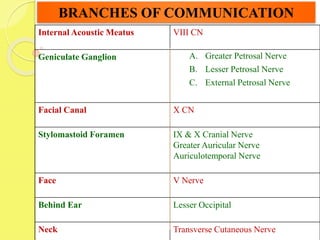
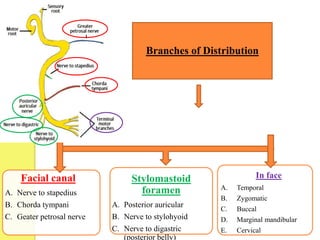
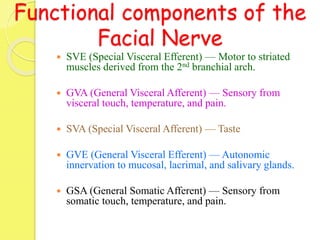
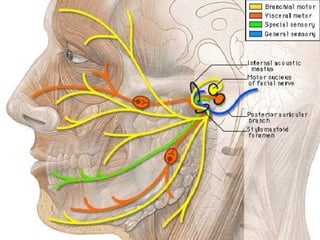
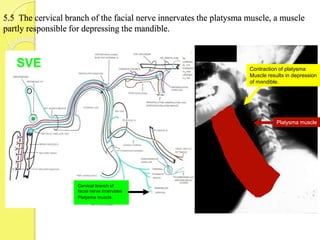
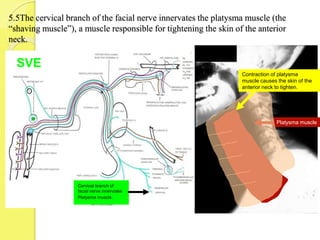
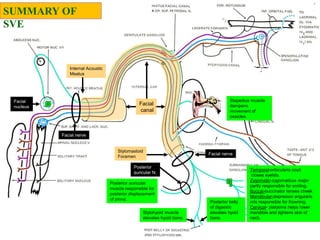
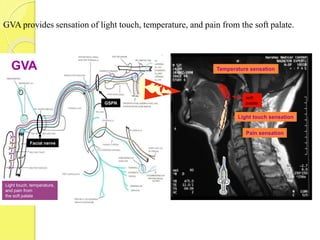
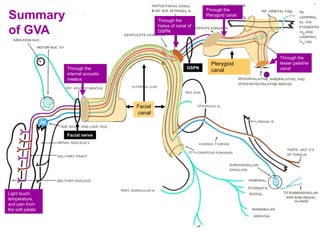
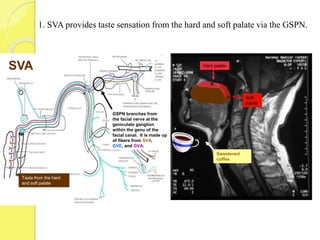
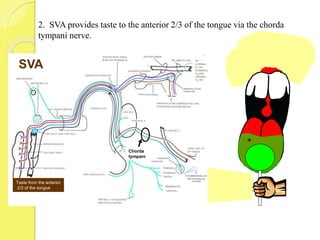
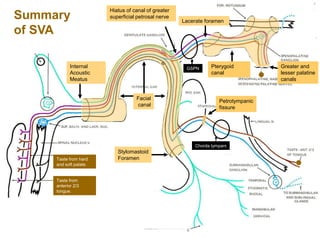
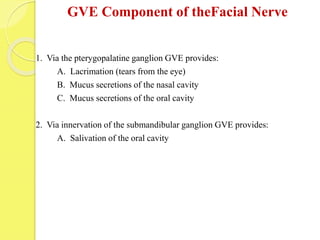
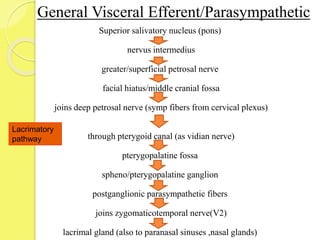
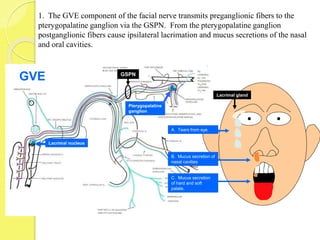
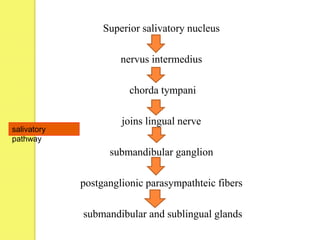
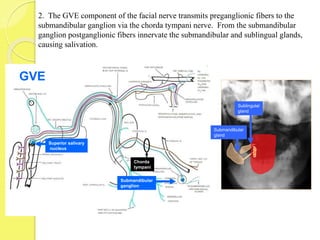
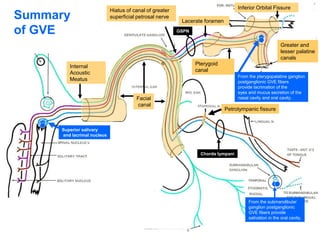
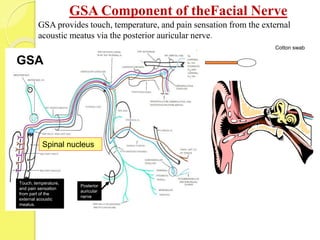
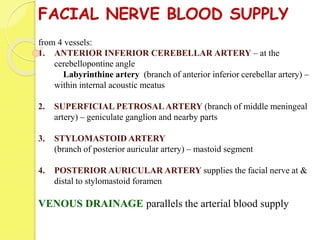
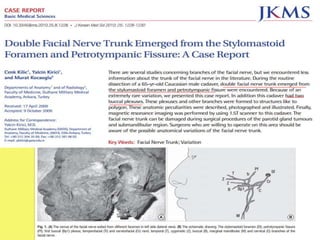
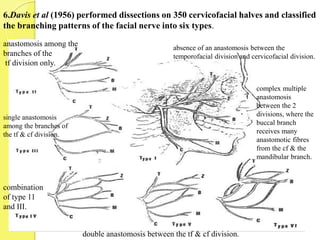
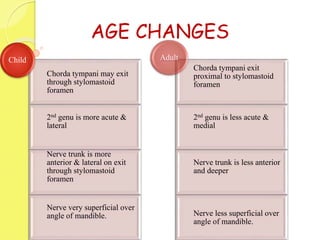
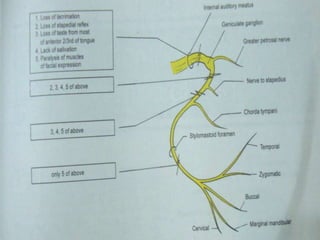
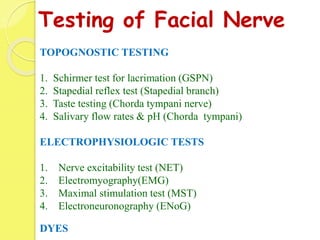
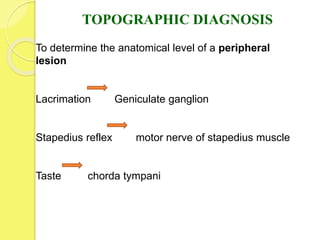
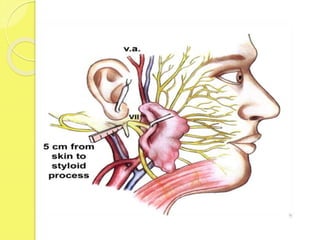
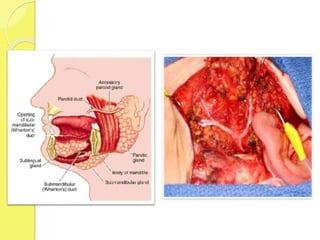
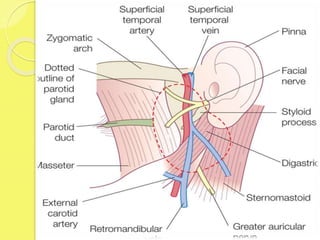
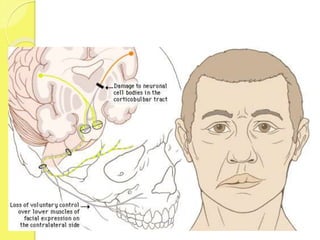
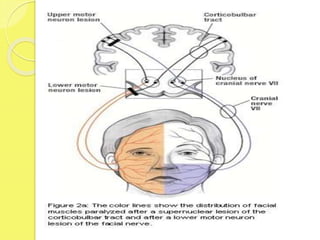
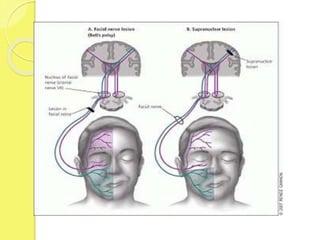
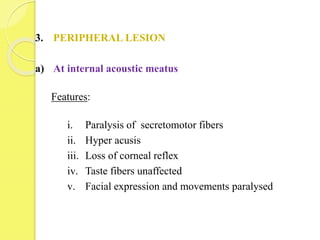
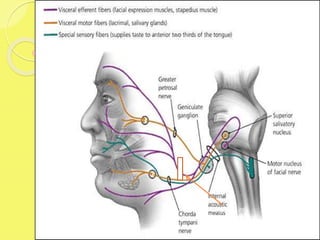
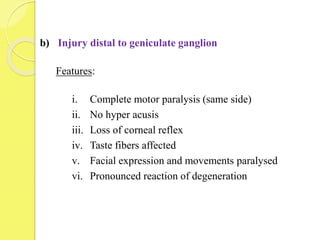
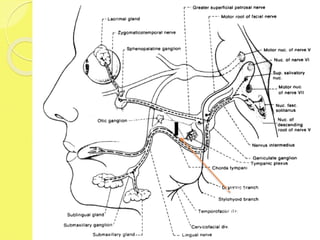
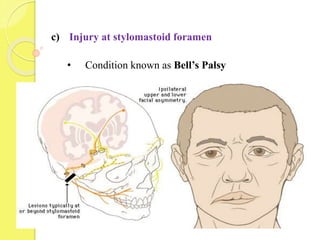
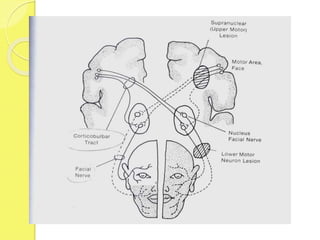
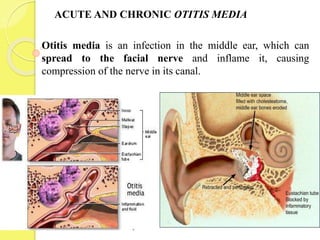
The facial nerve is a mixed nerve that originates in the brainstem and has multiple branches that innervate muscles of facial expression and provide motor, sensory, parasympathetic, and taste functions. It exits the skull through the internal acoustic meatus and stylomastoid foramen, giving off branches along its course like the chorda tympani nerve. The facial nerve has motor, sensory, parasympathetic, and special sensory components that allow for facial muscle movement and provide various sensory functions like taste.