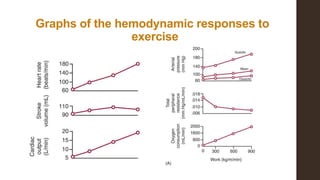
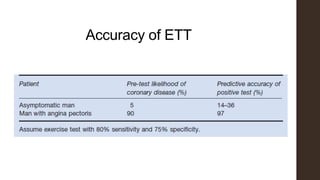
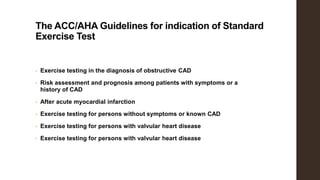
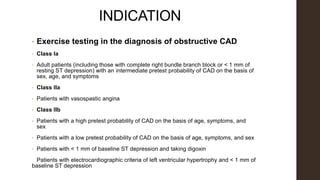
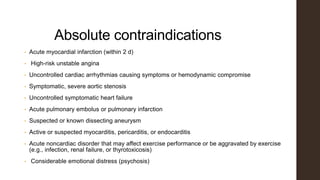
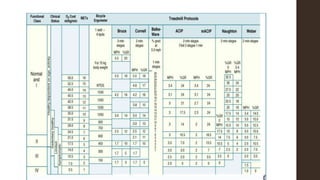
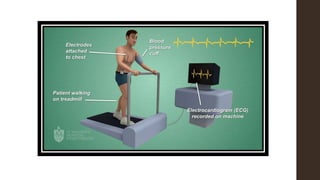
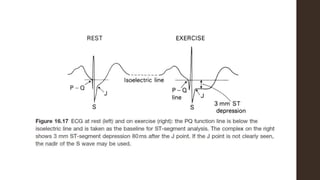
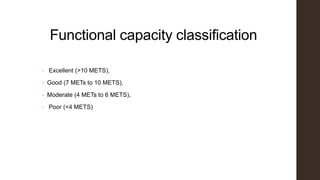
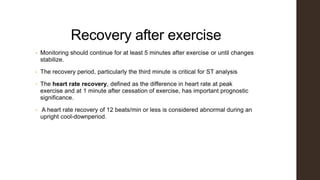
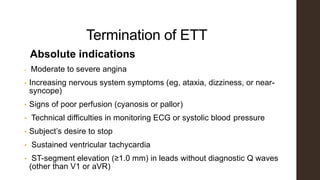
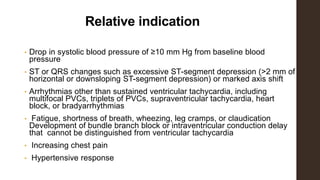
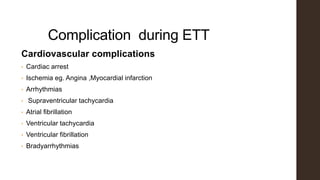
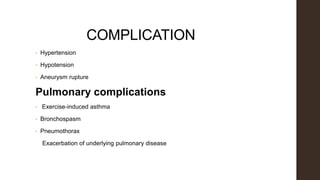
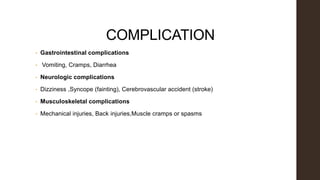
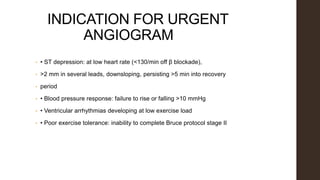
Exercise tolerance testing (ETT) is a noninvasive test that evaluates the cardiovascular system's response to exercise. It can help diagnose cardiac disease, assess prognosis, and evaluate treatment effects. The test monitors electrocardiogram, blood pressure, functional capacity, and symptoms during increasing levels of exercise. It has advantages of safety, availability, and low cost but has low sensitivity and specificity. Complications can include cardiac events, arrhythmias, and pulmonary issues.