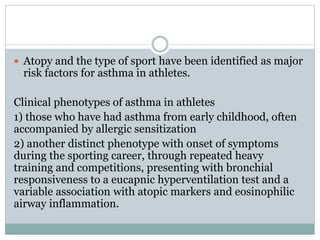
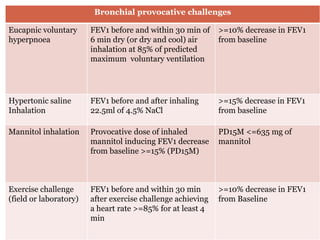
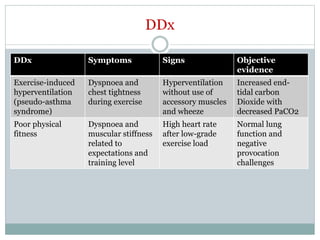
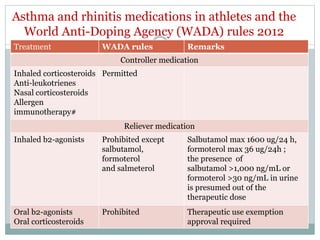
This document discusses exercise-induced asthma in athletes. It defines exercise-induced asthma and bronchoconstriction, and identifies risk factors like atopy and certain sports. It describes diagnostic methods and criteria used to document exercise-induced bronchoconstriction in athletes. Differential diagnoses are provided. Treatment involves both controller and reliever medications according to anti-doping regulations. Preventive strategies to reduce exercise-induced bronchoconstriction include allergen avoidance, immunotherapy, warm-up/cool-down exercises, nose breathing, and managing comorbidities.