[1] Ocular Surface Squamous Neoplasia (OSSN) refers to a spectrum of dysplastic and malignant squamous lesions of the conjunctiva and cornea.
[2] Diagnosis is usually clinical but can be confirmed with biopsy. For suspected OSSN less than 3 clock hours, excision biopsy with cryotherapy and alcohol epitheliectomy is performed. Larger lesions may require chemoreduction with topical chemotherapy prior to surgery and cryotherapy.
[3] Risk factors include ultraviolet light, HIV, and human papillomavirus. While rare, metastasis can occur to local lymph nodes or distant sites like lungs. Recurrence after treatment ranges from 15-52% depending
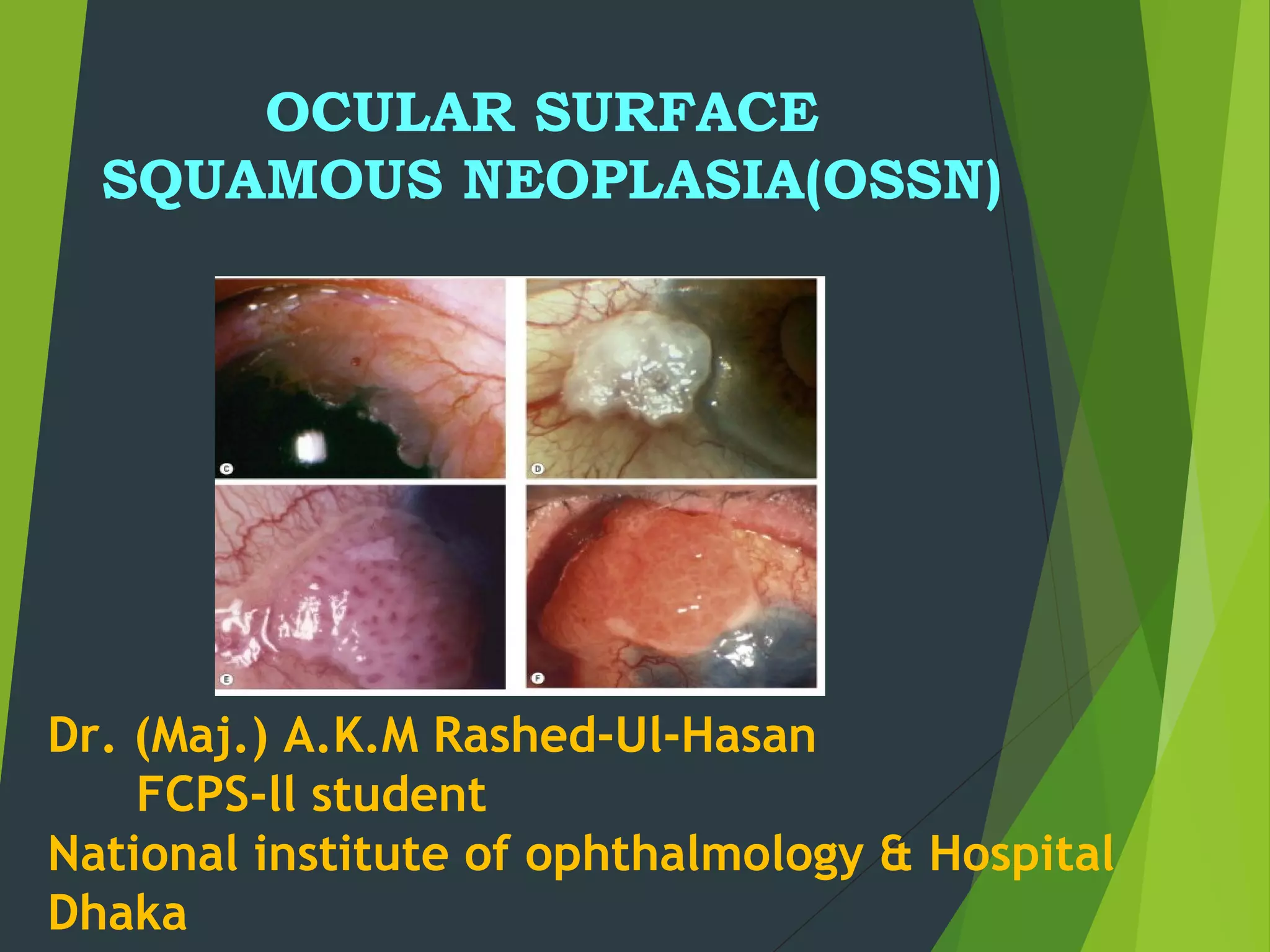

![Definition
The term Ocular Surface Squamous
Neoplasia [OSSN] presently refers to the
entire spectrum of dysplastic, pre-invasive
and malignant squamous lesions of the
conjunctiva and cornea](https://image.slidesharecdn.com/ocularsurfacesquamousneoplasia-160526135042/85/Ocular-surface-squamous-neoplasia-4-320.jpg)

































![SUMMARY
[1] Suspected OSSN < 3 clock hours
Excision biopsy +
base/ edge cryotherapy +
alchohol epitheliectomy is done.](https://image.slidesharecdn.com/ocularsurfacesquamousneoplasia-160526135042/85/Ocular-surface-squamous-neoplasia-38-320.jpg)
![[2] Suspected OSSN 3 – 6 clock hours –
A diagnostic biopsy is required
Pre-invasive lesions
topical chemotherapy
Invasive lesions
surgery + cryotherapy is done after
chemoreduction with 4 to 6 cycles of topical
chemotherapy.](https://image.slidesharecdn.com/ocularsurfacesquamousneoplasia-160526135042/85/Ocular-surface-squamous-neoplasia-39-320.jpg)
![[3] OSSN > 6 clock hours –
A diagnostic biopsy is
required.
Pre-invasive lesions
Topical chemotherapy
Invasive
Surgery + cryotherapy is done after
chemoreduction with 4 to 6 cycles of topical
chemotherapy.
If there is no response to chemotherapy
Palliative radiotherapy or extensive surgery like
enucleation / exenteration may be required.](https://image.slidesharecdn.com/ocularsurfacesquamousneoplasia-160526135042/85/Ocular-surface-squamous-neoplasia-40-320.jpg)



