This textbook examines diseases of the ear, nose and throat. It describes the anatomy, physiology, pathology and treatment of ENT diseases. The textbook provides both classic and modern scientific data on different branches of otorhinolaryngology. The textbook is intended for students at institutions of higher medical education studying ENT.
















































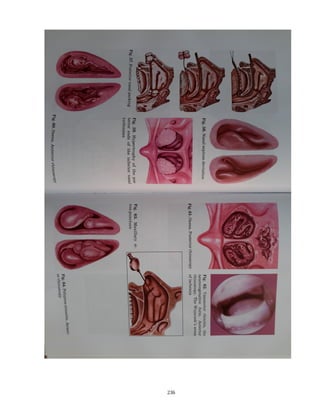
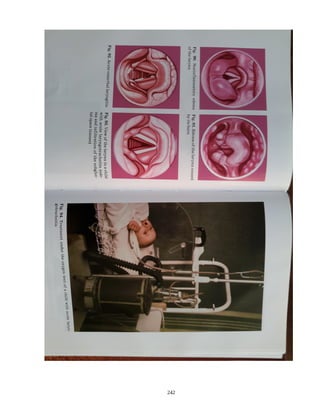
![diseases. During mesopharyngoscopy the physician takes a spatula with his left hand,
putting his right hand on the patient’s head and fixing it. The physician puts the
spatula on the anterior two thirds of the tongue and warily, slowly presses on the back
of tongue downwards. Strong pressure may cause vomiting. Mesopharyngoscopy
enables examination of the soft palate and its mobility, inspection of the uvula,
palatine arches, palatine tonsils, posterior and lateral walls of pharynx, root of tongue
(Fig. 68). Attention is paid to the color of pharynx mucosa, relief of the posterior
pharyngeal wall surface, presence of lymphoid tissue mass in the form of granules or
lateral lines. There are detected such diseases of this part: abscesses, tumors,
extraneous bodies, etc.
Examination of the palatine tonsils detects their dimensions, palatine arches,
determines if their fusion with the tonsils, presence and character of content in the
lacuna. For detection of lacuna content it is necessary to press with a spatula on the
anterior palatine arch; the free surface the tonsil hidden behind the palatine arch can
also be examined.
In order to assess soft palate mobility one offers the examined person to
pronounce the sound [a].
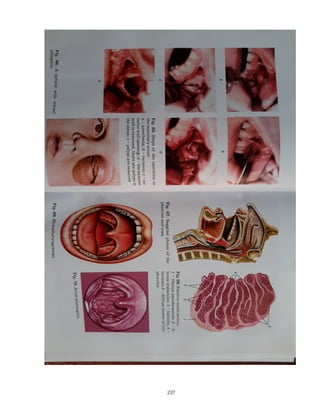
One can examine a larger area of the inferior pharynx part, lingual tonsil and
sometimes (especially in children) superior margin of epiglottis by firm pressure on
the root of tongue downwards. Yet more detailed examination of the laryngopharynx
is provided by using a laryngeal mirror, like in case of laryngoscopy.
Hypopharyngoscopy is conducted, using laryngeal mirrors having a diameter of 19,
15, 25 mm. In the mirror one can see reflection of such structures as the root of
tongue, free margin of epiglottis, piriform recesses, posterior and lateral walls of
laryngopharynx and its transition to the esophagus. Examination of the inferior part
pharynx both in children and adults is also conducted during direct laryngoscopy.
If diphtheric incrustation is found, its bacteriologic study is conducted; if
leptotrichosis is suspected – one carries out bacterioscopy. When a malignant
114](https://image.slidesharecdn.com/entbook-160122174538/85/Ent-book-114-320.jpg)



























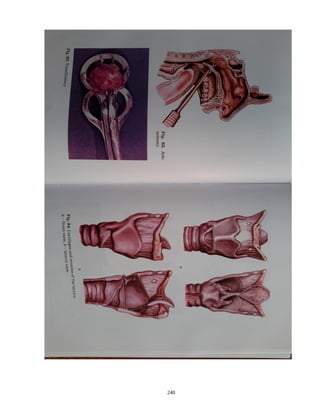
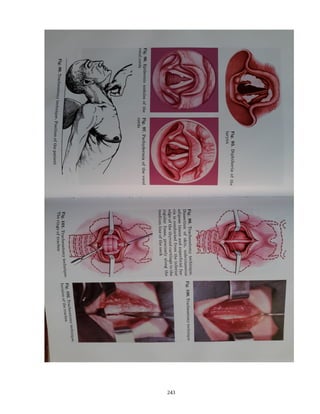
![The laryngeal mirror is taken in the right hand, the proglossis is held in a napkin
with two fingers of the left hand, and the index finger moves to the upper lip of the
patient. The mirror is brought into the mouth cavity and fixed against the soft palate. It
is not advisable to touch the root of tongue and posterior wall of gullet with the mirror,
it can cause vomiting. The research is conducted on condition of clear breathing,
phonation of the sounds [i] or [e] and deep breath. During indirect laryngoscopy the
state of the mucous tunic of larynx, form and dimensions of the glottis, mobility of the
larynx during phonation, state of the subglottal space and superior part of trachea are
estimated.
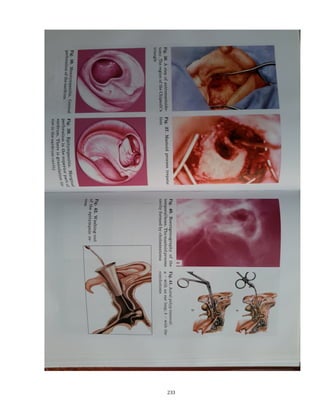
If indirect laryngoscopy is impossible, direct laryngoscopy is conducted (Fig.
87). Indications to direct laryngoscopy are: 1) examination of the larynx in younger
children and also in adults if detailed indirect laryngoscopy is not successful; 2)
endolaryngeal interferences, which can not be conducted at mirror laryngoscopy due to
their considerable duration and complexity; 3) introduction of an intratracheal tube or a
bronchoscope cone into the trachea; 4) examination and maneuvers in the hypopharynx
and the area of the opening in gullet; 5) bronchoscopy.
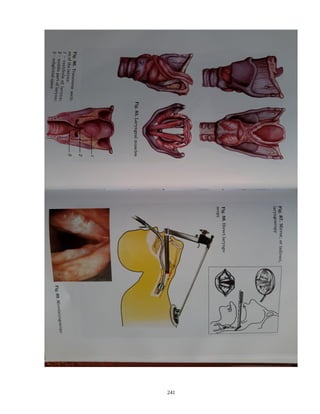
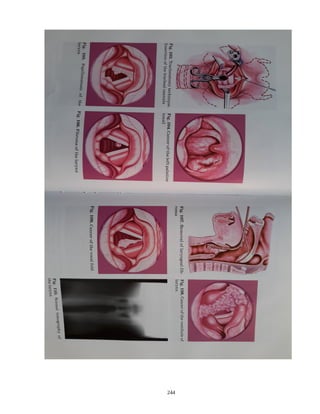
The method of direct laryngoscopy consists in straightening of the angle between
the mouth cavity and the gullet with the laryngoscope blade, which allows examining
the larynx and trachea. All laryngoscopes used in otorhinolaryngology can be divided
into two groups:
1) laryngoscopes kept in the doctor’s hand during direct laryngoscopy;
2) laryngoscopes introduced into the larynx and fixed, due to what the hands of the
doctor conducting manipulation remain free; this type of laryngoscopy is named
suspension or support.
Microlaryngoscopy is the research of the larynx with an operating
microscope with the focal distance of 300–400 mm (Fig. 88). This research can be
conducted both at mirror and direct laryngoscopy. On the basis of microlaryngoscopy
the microsurgery of larynx developed.
159](https://image.slidesharecdn.com/entbook-160122174538/85/Ent-book-159-320.jpg)