The document provides an overview of basic endoscopic equipment, including:
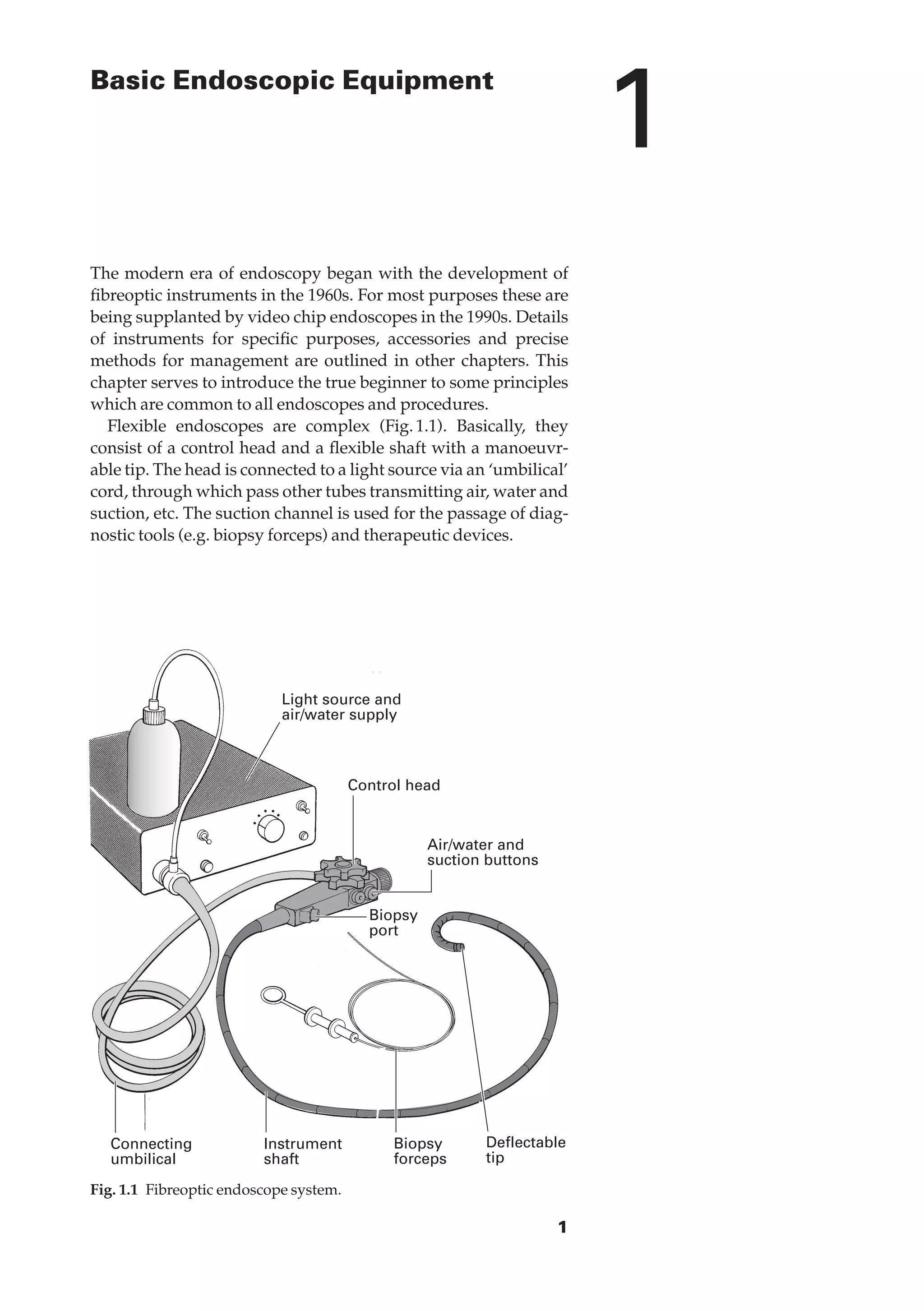
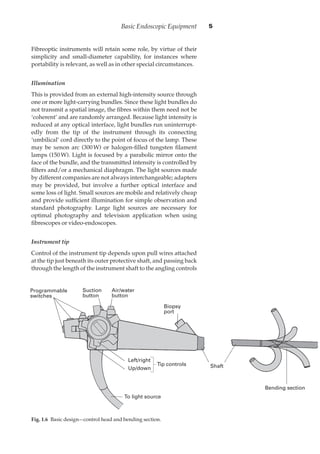
- Flexible endoscopes consist of a control head connected via umbilical cord to a light source, with tubes transmitting air, water, and suction, and a suction channel for diagnostic and therapeutic devices.
- Fibreoptic endoscopes transmit images via tightly packed bundles of glass fibers, providing flexibility but lower image quality than rigid lenses.
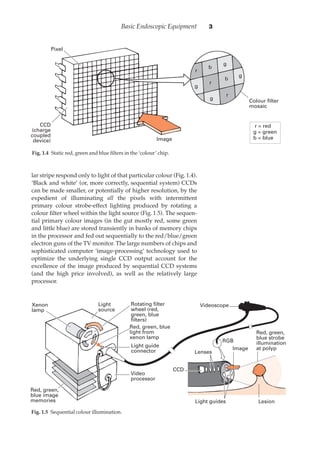
- Video endoscopes use a CCD chip at the tip instead of an optical bundle, allowing digital images and simultaneous viewing without quality loss.
- Proper illumination is crucial and provided by external light sources transmitted via light bundles to the tip.