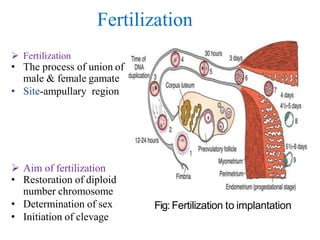
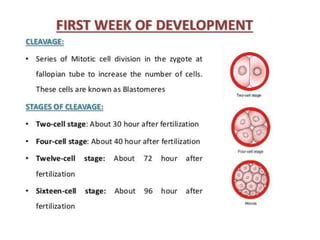
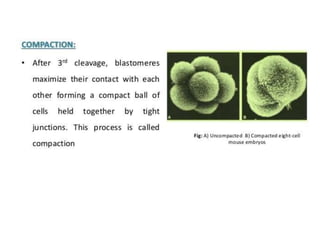
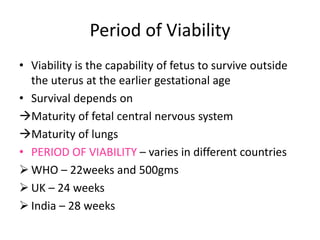
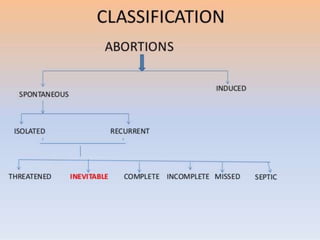
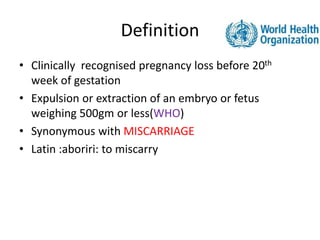
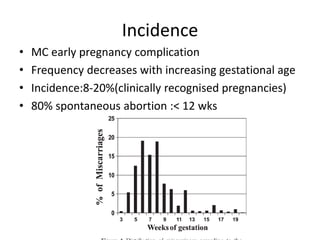
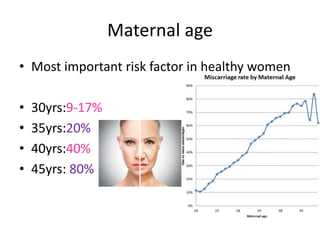
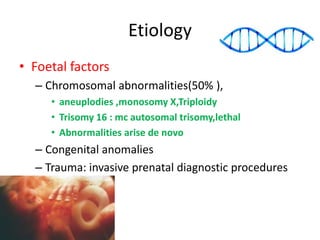
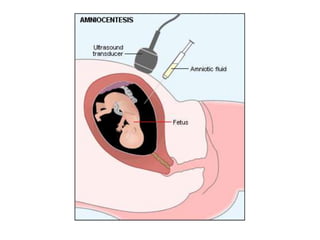
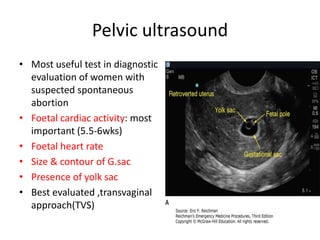
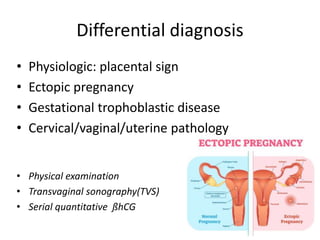
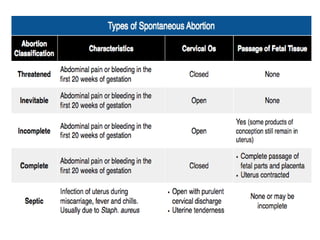
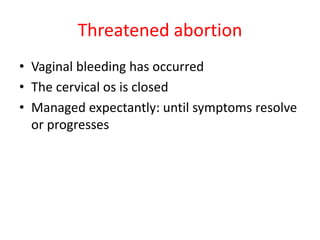
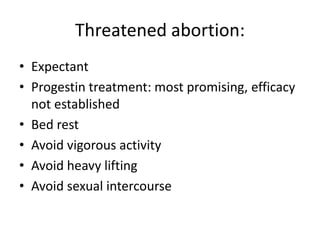
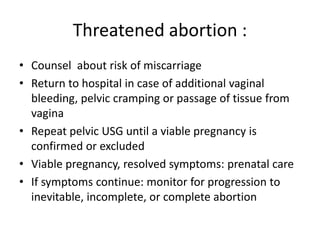
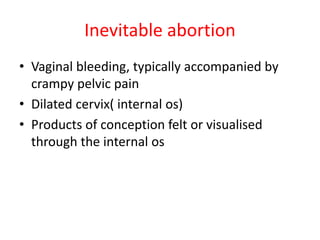
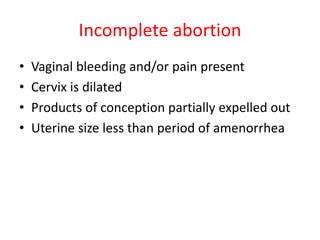
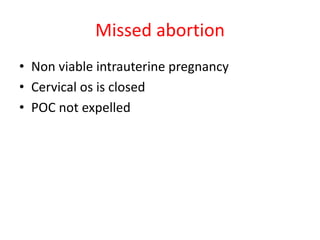
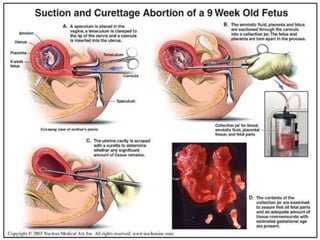
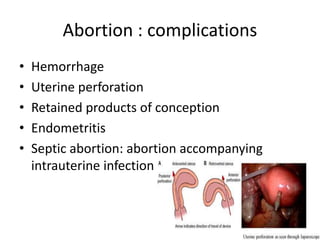
The document discusses fertilization, the period of viability for fetuses, and spontaneous abortion, which is clinically recognized pregnancy loss before the 20th week of gestation. It outlines the definition, incidence, risk factors, clinical presentation, diagnostic evaluation, and management of spontaneous abortion, noting key predictors and interventions. It emphasizes the importance of preconception and prenatal counseling to manage modifiable risk factors that can lead to pregnancy losses.