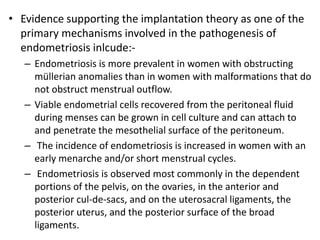
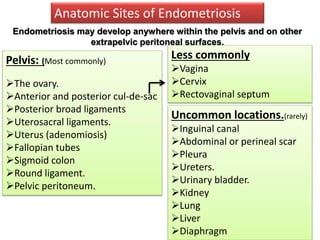
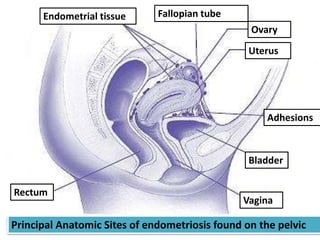
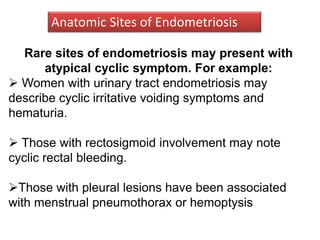
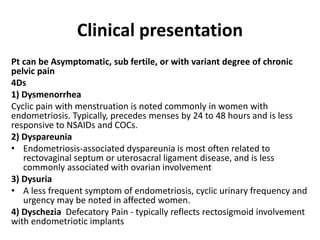
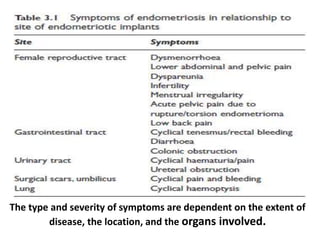
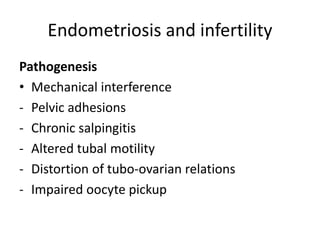
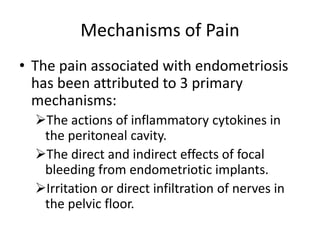
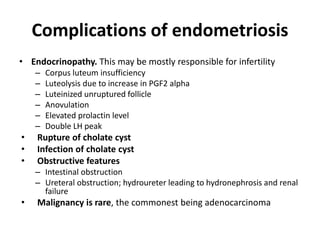
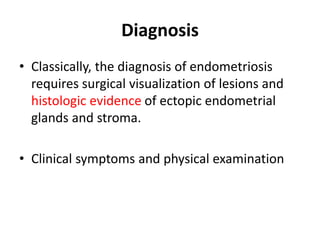
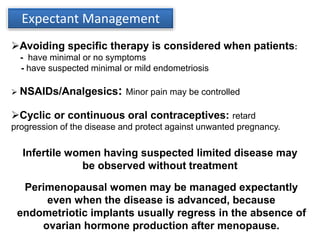
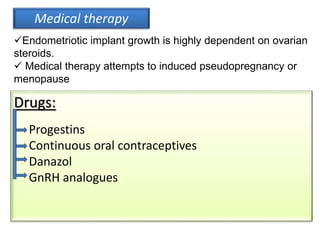
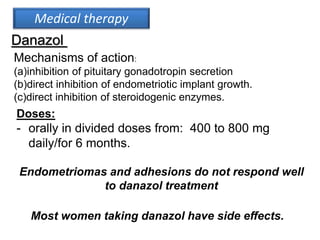
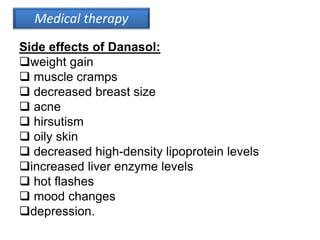
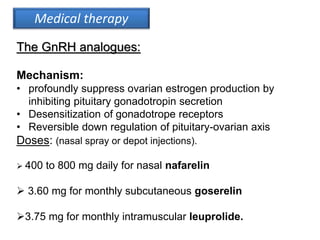
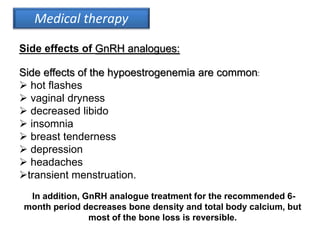
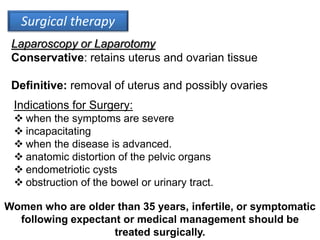
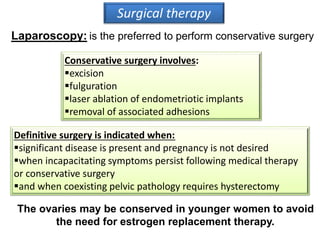
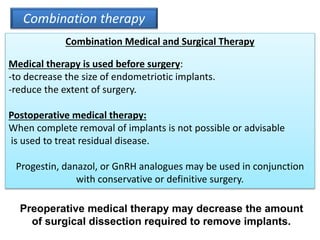
Endometriosis is a condition where endometrial tissue grows outside the uterine cavity, most commonly on the ovaries and pelvic peritoneum. It causes pelvic pain and infertility and is diagnosed through laparoscopy. Treatment involves medical therapy using hormones to suppress menstruation, surgical excision or ablation of lesions, or a combination. Symptoms range from mild to severe depending on location and extent of disease.