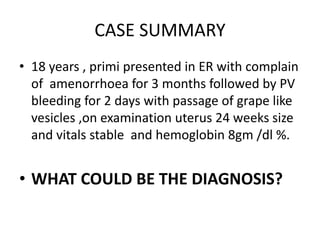
The document discusses a case of a 18-year-old female presenting with symptoms of amenorrhea followed by vaginal bleeding and grape-like vesicles, leading to a diagnosis of molar pregnancy, a type of gestational trophoblastic disease (GTD). It details the definition, incidence, types, clinical features, diagnosis, management options, and complications associated with GTD. Key findings include the various treatments based on risk scoring and the significance of monitoring hCG levels post-management.