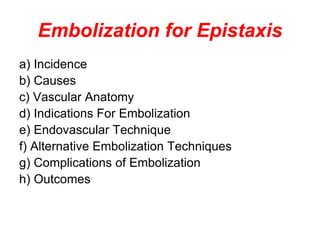
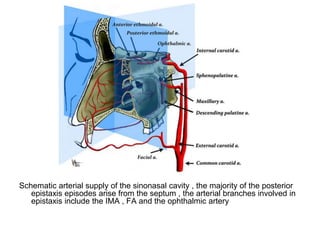
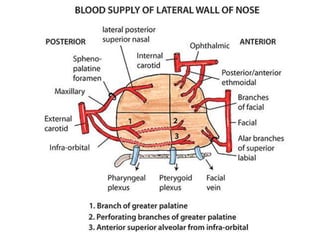
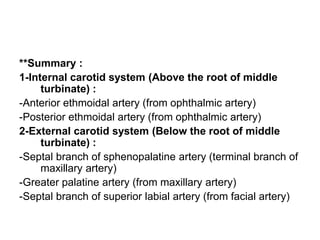
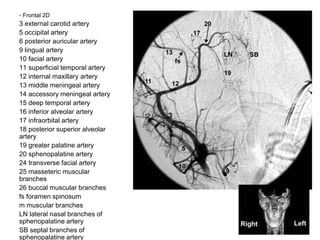
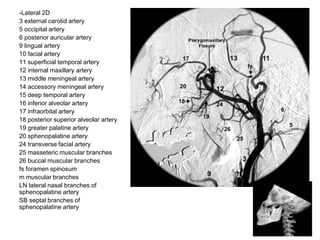
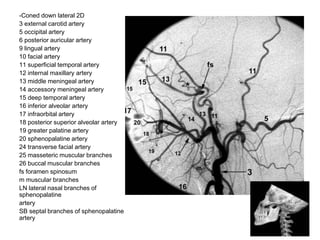
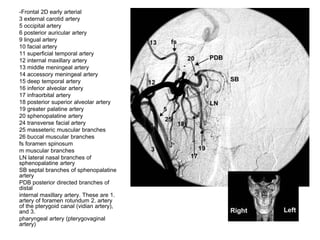
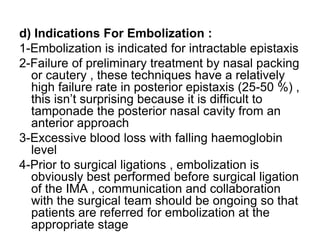
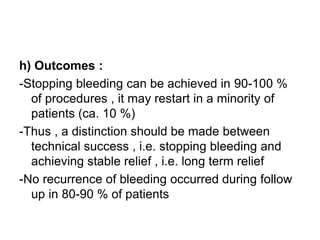
1. The document discusses interventional neuroradiology techniques for embolization to treat epistaxis. It covers the vascular anatomy of the nose, indications for embolization when nasal packing and cautery fail, and the endovascular technique for embolization.
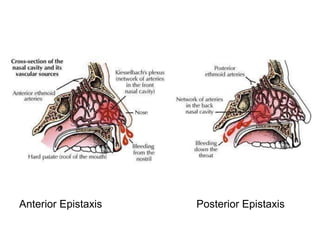
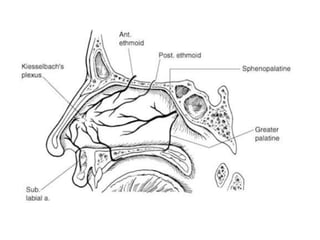
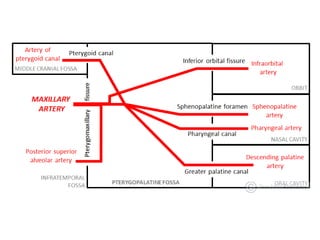
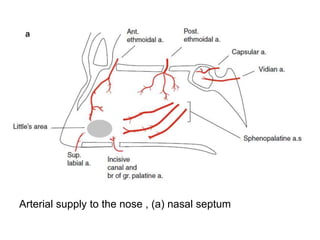
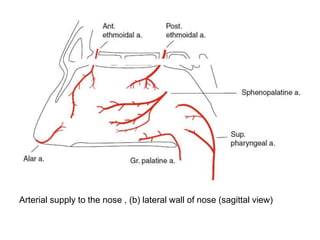
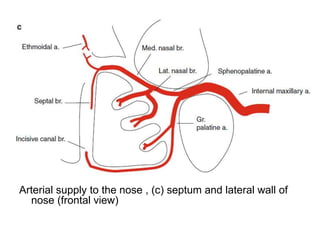
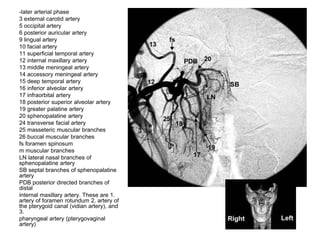
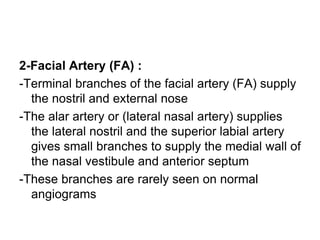
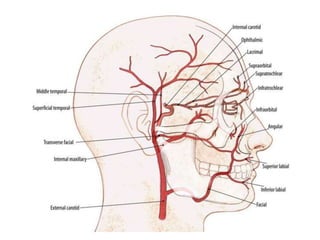
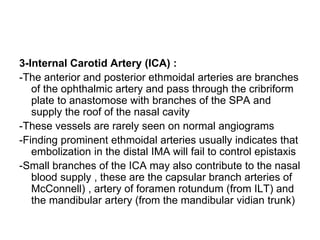
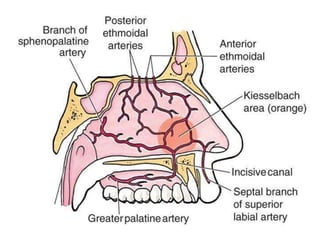
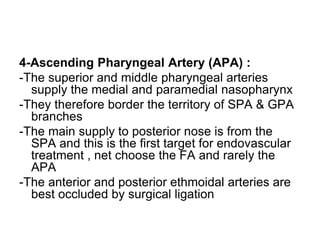
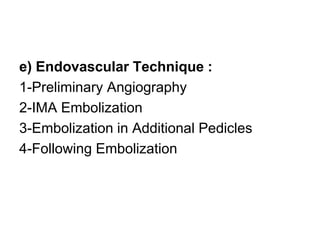
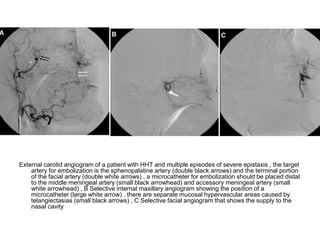
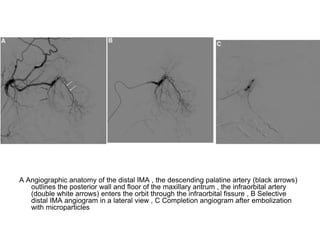
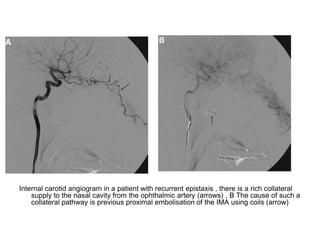
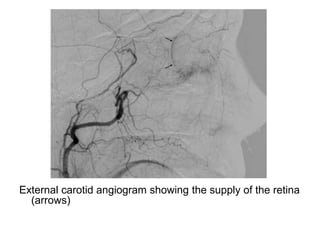
2. The technique involves preliminary angiography of the internal and external carotid arteries to identify blood supply, followed by selective catheterization of the internal maxillary artery to embolize its branches supplying the nose, particularly the sphenopalatine artery.
3. Particle embolization is performed to occlude the arterial supply, using initially smaller particles followed by larger ones for complete occlusion. This cuts off the primary blood supply to the nasal