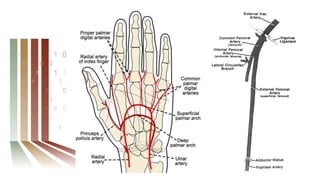
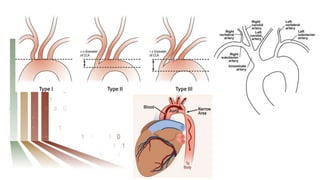
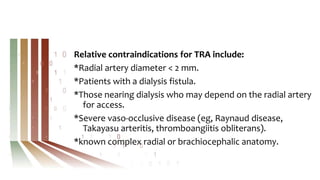
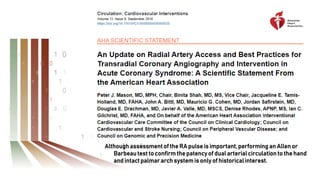
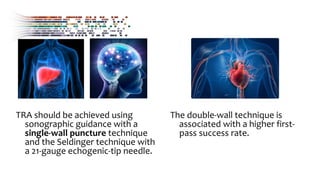
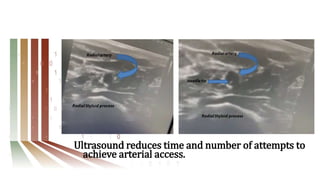
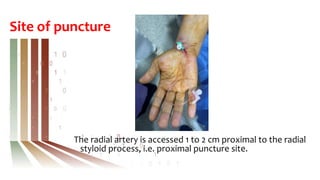
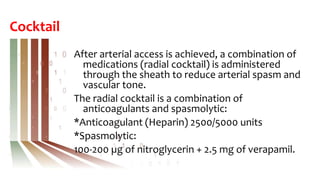
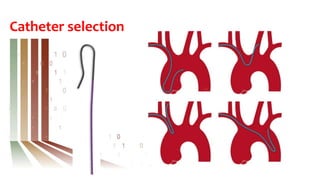
This document provides an introduction and overview of the transradial approach for neurointerventions. It discusses why the radial approach is preferable to the femoral approach, including lower bleeding risks and access site complications. It covers topics like assessing the radial artery, achieving arterial access using ultrasound guidance, administering a "radial cocktail" of medications, challenges that can be encountered, achieving hemostasis, and potential complications. The conclusion recommends embracing the radial approach as it offers safety benefits and improved patient outcomes and satisfaction compared to the traditional transfemoral approach.