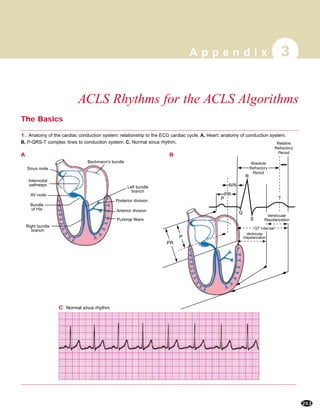
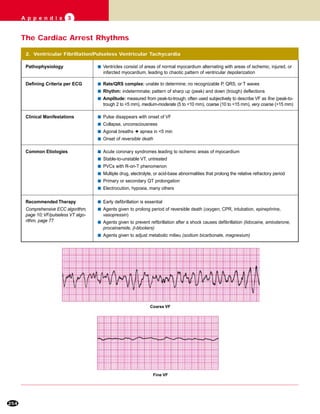
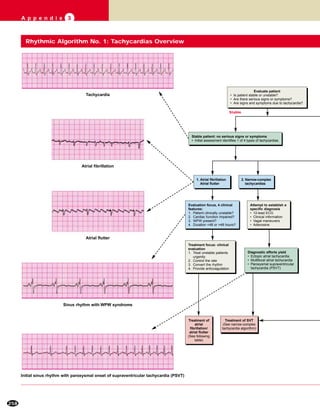
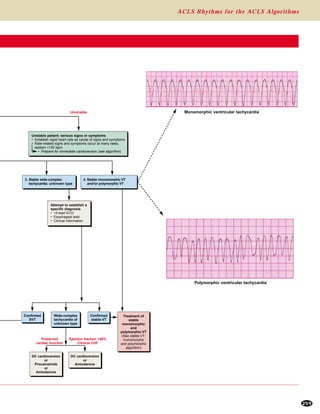
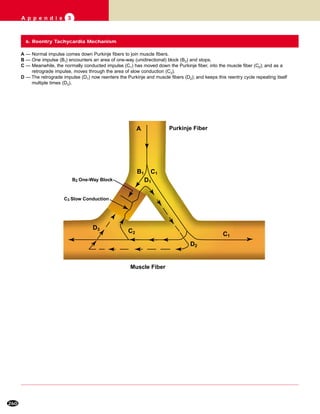
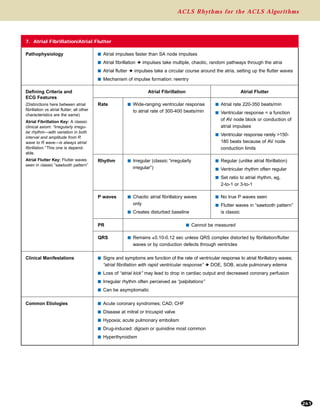
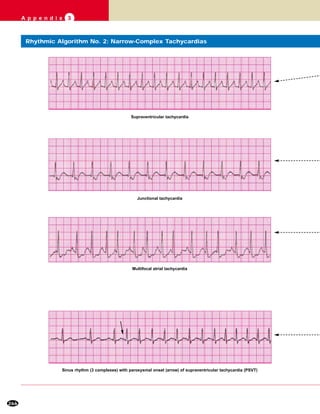
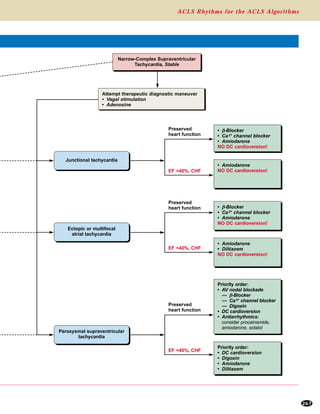
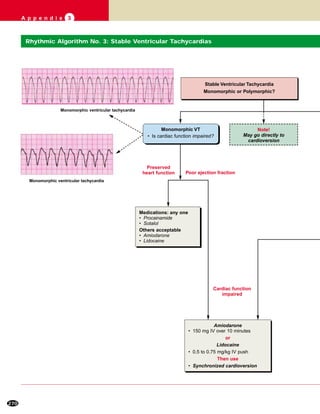
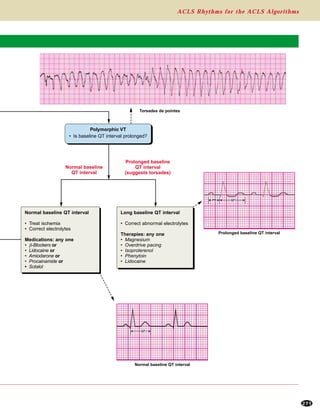
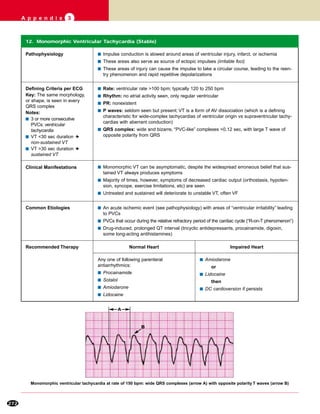
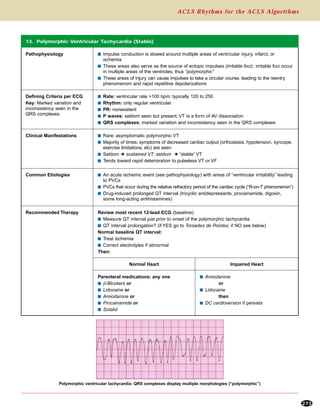
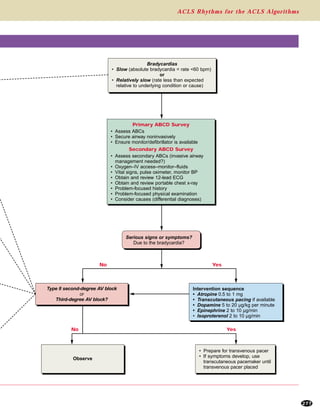
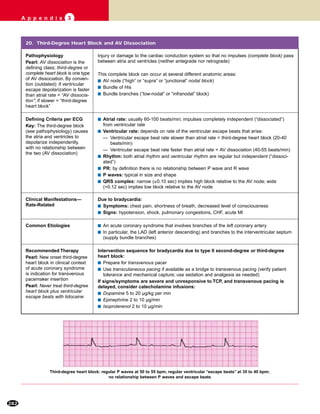
This document provides information on cardiac rhythms that may be encountered in advanced cardiac life support (ACLS). It begins with an overview of cardiac anatomy and the normal cardiac conduction system. It then describes the pathophysiology, clinical manifestations, common causes, and treatment recommendations for several cardiac rhythms including ventricular fibrillation/pulseless ventricular tachycardia, pulseless electrical activity, asystole, sinus tachycardia, atrial fibrillation/flutter, Wolff-Parkinson-White syndrome, and reentry tachycardia mechanism. For each rhythm, it provides the defining electrocardiogram criteria, clinical implications, and treatment algorithm.