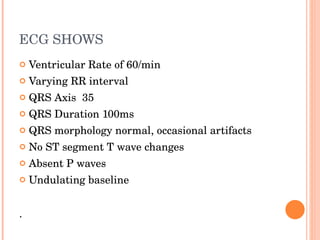
A 65-year-old lady presented with breathlessness and was found to have an irregularly irregular pulse. Her ECG showed atrial fibrillation with a slow ventricular response of 60 beats per minute and no P waves. She was diagnosed with new onset atrial fibrillation. As it appeared to be ongoing for more than 48 hours, she would be anticoagulated. An echocardiogram and further testing were planned to evaluate for underlying structural heart disease or clots that may have increased her risk of stroke.