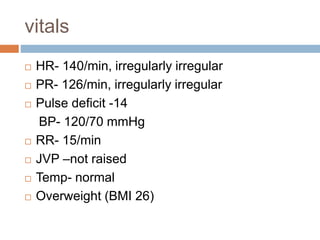
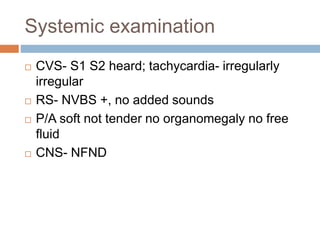
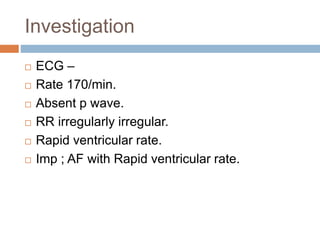
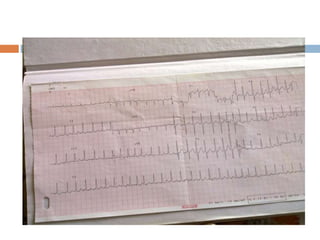
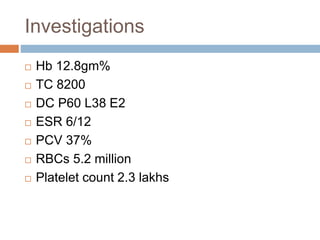
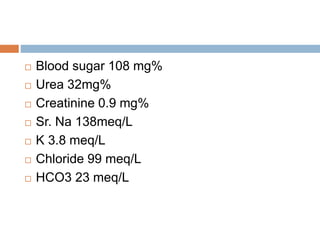
A 28-year-old female presented with episodic palpitations for 3 months along with chest pain and weight gain. On examination, she was found to have an irregularly irregular heart rate of 140 bpm. An ECG showed atrial fibrillation with a rapid ventricular rate. Laboratory tests found hypothyroidism. She was started on medication for rate control and thyroid replacement. Her atrial fibrillation converted to normal sinus rhythm after one week of treatment. Hypothyroidism can cause atrial fibrillation due to effects on the heart and literature reports cases of hypothyroidism-induced atrial fibrillation.
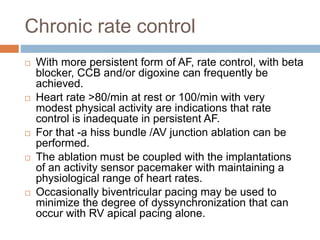
![Catheter and surgical ablative
therapy to prevent recurrent AF
Most ablation strategies incorporate techniques that isolate an atrial
muscle sleeves entering the pulmonary veins.
Patient with recurrent symptomatic AF, because of by this procedure
, elimination of AF is 50-80%.
Risk related to left atrial ablation procedure albeit low[over all 2-4
%], include pulmonary vein stenosis, atrio esophageal fistula,
systemic embolic event & perforation/tamponade.
Surgical ablation usually performed at the time of other cardiac
valve or coronary artery surgery & less commonly as a stand alone
procedure.
The cox surgical maze procedure is designed to interrupt all macro
re entrant circuits that might potentially develop in the atria thereby
precluding the ability of the atria to fibrillate.
The multiple incisions of the traditional cox maze procedure have
been replaced with linear lines of ablation, and pulmonary vein
isolation using a variety of energy sources](https://image.slidesharecdn.com/anunusualpresentationofcommondisorder-101027080932-phpapp01/85/Atrial-Fibrillation-in-Hypothyroidism-37-320.jpg)