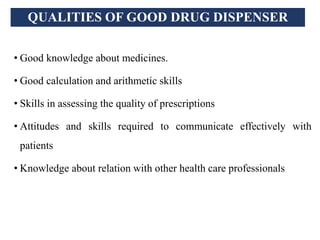
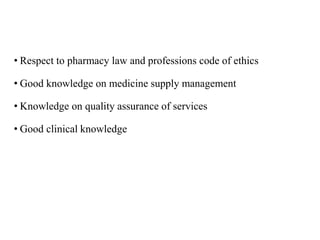
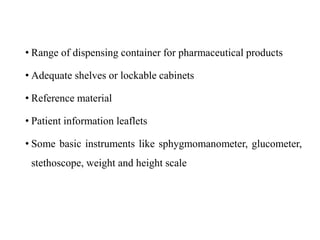
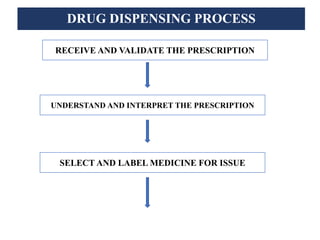
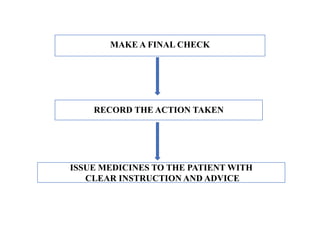
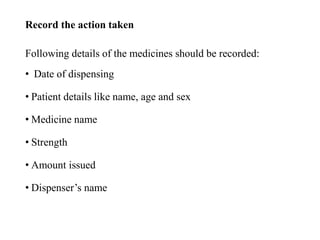
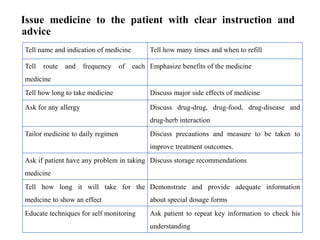
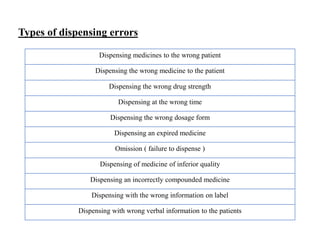
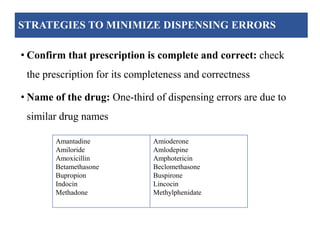
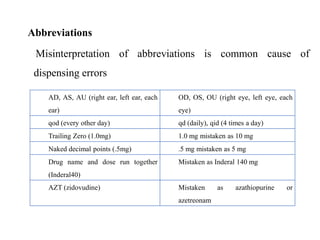
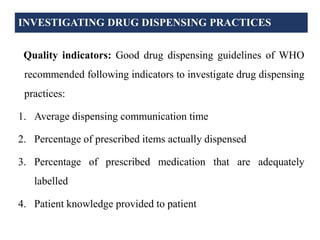
The document discusses drug dispensing practices, emphasizing the importance of effective dispensing for rational medicine use. It outlines the essential roles and qualities of dispensers, the environment needed for good dispensing, and processes to minimize dispensing errors. Additionally, it highlights strategies for quality improvement in drug dispensing and the significance of well-trained personnel in ensuring safe medication distribution.