This document discusses medication errors, including their causes, types, where they occur in the medication process, and strategies to improve safety. Key points include:
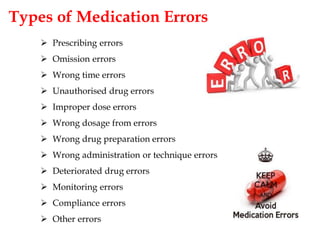
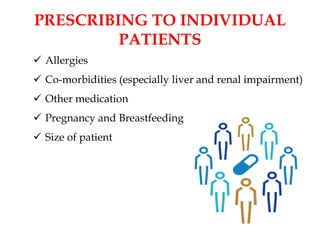
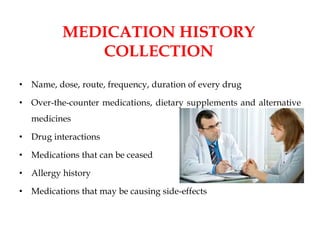
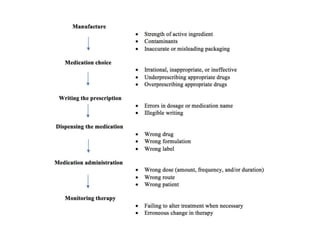
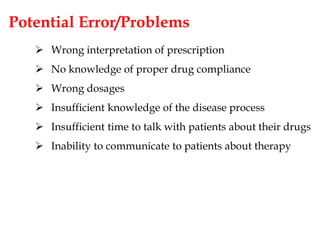
- Medication errors can happen at various stages from prescribing to administration and are caused by factors like multiple drug usage and prescribers.
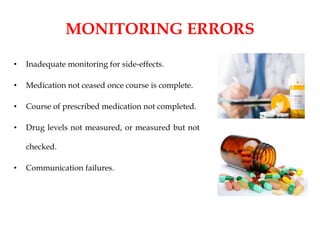
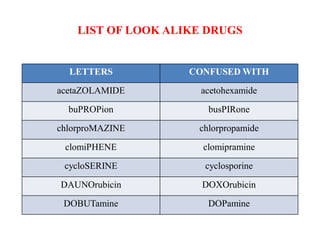
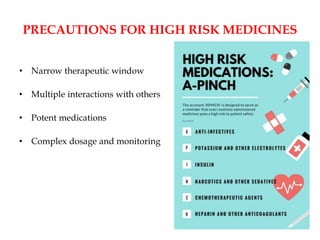
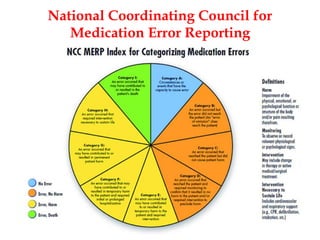
- Errors include wrong dosages, omitting drugs, and monitoring issues. High alert drugs require special precautions.
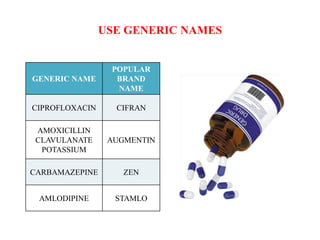
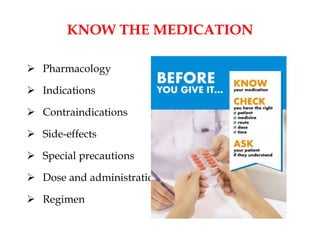
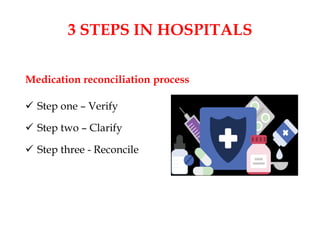
- Improving safety involves clear communication, checking practices, reporting errors to learn from them, and using technology tools and multidisciplinary teams.
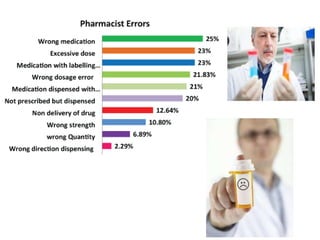
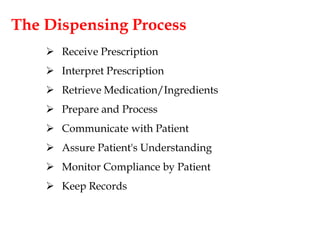
- Pharmacists can help by implementing systems like unit dose distribution and providing education. Overall a systematic approach is needed to examine issues and implement changes.