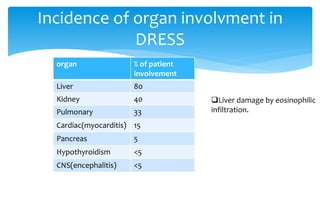
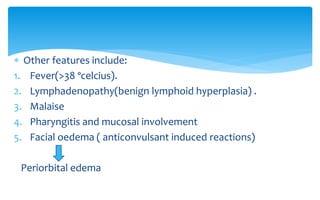
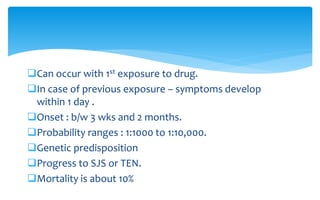
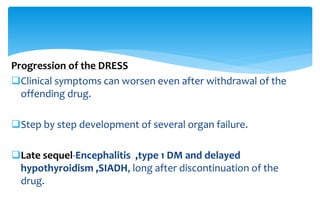
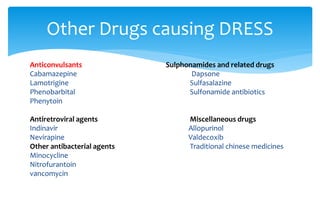
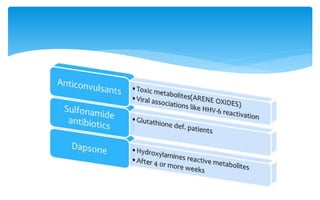
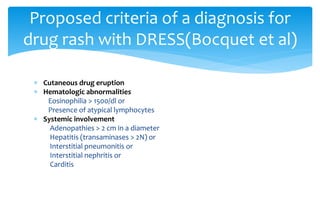
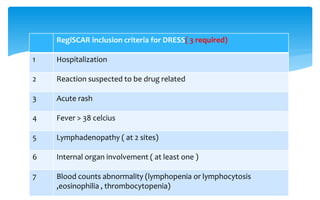
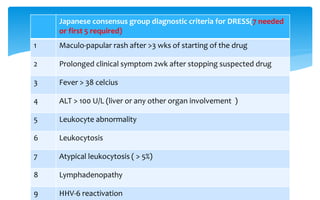
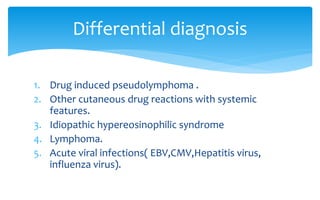
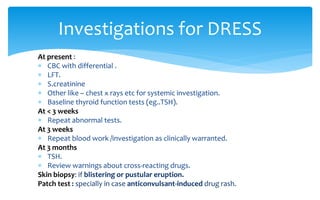
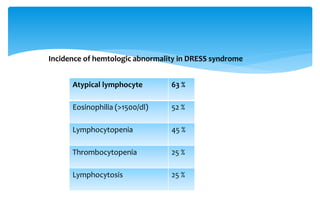
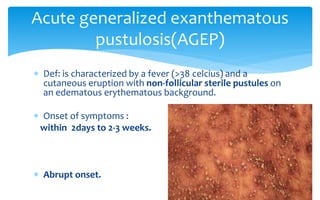
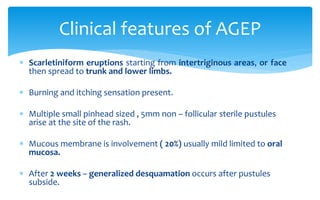
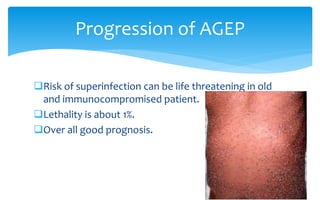
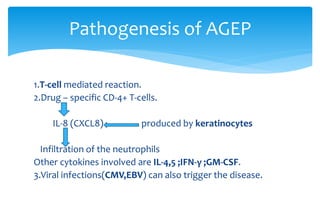
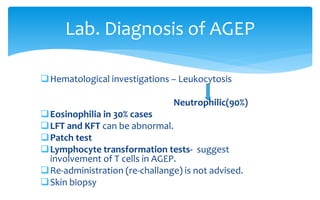
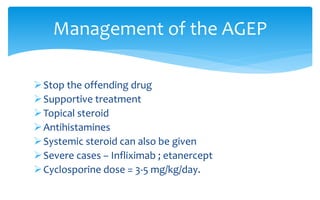
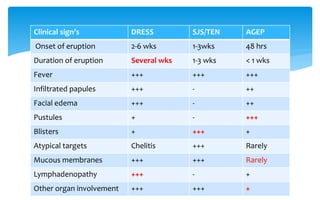
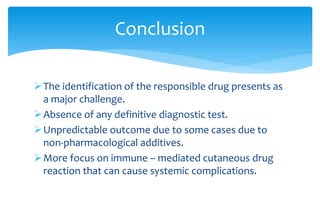
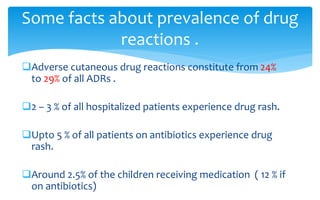
The document discusses two types of adverse cutaneous drug reactions: drug reaction with eosinophilia and systemic symptoms (DRESS) and acute generalized exanthematous pustulosis (AGEP). DRESS is characterized by a skin eruption, hematologic abnormalities like eosinophilia, and internal organ involvement. It has a delayed onset and can cause long-term complications. AGEP presents with sudden onset of fever and a pustular rash, but does not involve internal organs. Both can be life-threatening but typically resolve after stopping the culprit drug.
![ Defination: is a severe cutaneous event characterized by a
Triad of :
1. Skin eruptions ,
2. Hematologic abnormalities[hypereosinophilia(80%) and atypical
lymphocytes/mononucleosis (40%)],
3. Internal organ involvement( Acute and Late sequelae) .
Heterogenesity of the initial presentation leads to it’s
misdiagnosis as infection .
Drug reaction with eosinophilia and
systemic symptoms (DRESS).](https://image.slidesharecdn.com/dr-140608010529-phpapp01/85/DRESS-AND-AGEP-13-320.jpg)