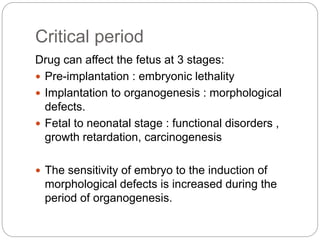
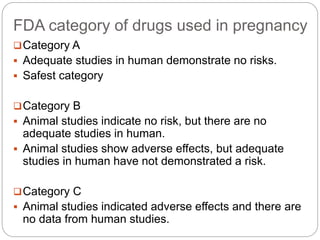
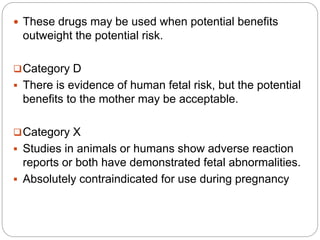
This document discusses teratogenicity studies and provides details on how to conduct prenatal developmental toxicity tests according to OECD Guideline 414. It defines key terms like teratogen and teratology. Historical teratogens like thalidomide, Accutane, DES, and alcohol are described along with their effects. The FDA pregnancy drug categories and critical periods of development are outlined. Test procedures include selecting animal species, housing, dosing, observations, post-mortem examinations of dams and fetuses, and results reporting. The goal is to identify effects of substances on prenatal development and discriminate between general toxicity and developmental toxicity.
![Accutane [isotetrinoin]
• It is used to treat acne.
• Birth defects : facial malformation, heart defects,
mental retardation.
Diethylstilbesterol [DES]
• From 1940 to 1970 ,DES was used to help maintain
pregnancy.
• Women who were exposed in utero often developed
vaginal neoplasia, vaginal adenosis, and cervical
erosion.
• Effects were not seen in offspring until they reach
puberty.](https://image.slidesharecdn.com/doc-20220404-wa0001-230426081540-2dcfd047/85/DOC-20220404-WA0001-pptx-6-320.jpg)
![Alcohol
• Heavy drinking during the early pregnancy greatly
increases the risk of cluster of birth difects known as
fetal alcohol syndrome.
o Fetal alcohol syndrome :
• This syndrome includes a small skull [microcephaly],
abnormal facial features, and heart defects, often
accompined by impeded growth and mental
retardation.
• Signs and symptoms : poor body weight, poor
memory, learning disabilities, speech and language
delay, difficulty with attension.](https://image.slidesharecdn.com/doc-20220404-wa0001-230426081540-2dcfd047/85/DOC-20220404-WA0001-pptx-7-320.jpg)
![Post-mortem examination
Females should be killed one day prior to the
expected day of delivery.
At the time of termination or death during the study,
the dam should be examined macroscopically for any
structural abnormalities or pathological changes.
Examination of uterine contents
Uteri that appear non-gravid should be further
examined [ ammonium sulfide staining for rodents and
Salewski staining for rabbit] to confirm non-pregnant
status.
Gravid uteri including the cervix should be weighed.](https://image.slidesharecdn.com/doc-20220404-wa0001-230426081540-2dcfd047/85/DOC-20220404-WA0001-pptx-17-320.jpg)