Tuberculosis (TB) is a chronic disease caused by the bacterium Mycobacterium tuberculosis. The document summarizes TB treatment guidelines including:
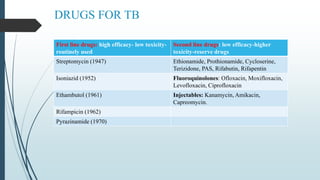
1) First-line drugs like isoniazid, rifampicin, pyrazinamide, and ethambutol are used for routine drug-sensitive TB treatment. Fixed-dose drug combinations and directly observed therapy (DOT) are recommended to ensure adherence.
2) Treatment duration is typically 6 months, or 9 months for cavitary disease. Treatment involves an intensive initial phase and continuation phase.
3) Special considerations are given for TB in children, pregnant/lactating women, HIV patients, and drug-resistant TB which require























![TB IN CHILDREN
There is an increasing trend of TB cases among children in Malaysia. AntiTB drug and
management of children with TB Suld be in line with the WHO Stop TB Strategy, taking
into consideration the epidemiology and clinical presentation of TB in children.
TB IN PREGNANT WOMEN
The WHO and British Thoracic Society consider H, R, E and Z to be safe to the foetus and
recommend the standard 6 month (2HRZE + 4HR) regimen for pregnant women with TB.
S is contraindicated because it is ototoxic to the foetus.
[Isoniazid (H), Rifampin (R), Pyrazinamide (2), Ethambutol (E)]](https://image.slidesharecdn.com/tb-230504152632-6986cab4/85/TB-pptx-29-320.jpg)
![Tuberculosis in lactation
Breast feeding mothers with TB should receive a full course of anti-TB drugs.
First-line anti-TB drugs are safe in breast feeding.
Mother and baby should stay together for continuation of breastfeeding. Once
active TB in the baby is ruled out, the baby should be given six months isoniazid
prophylaxis, followed by BCG vaccination.
Tuberculosis in AIDS patients
The association of HIV and TB infection is a serious problem. HIV positive
cases have a higher incidence of extrapulmonary, more severe, more lethal and
more infectious TB.
Initial intensive phase therapy with daily HRZE for 2 months is started
immediately on the diagnosis of TB, and is followed by a continuation phase of
HR for 4-7 months (total 6-9 months).
[Isoniazid (H), Rifampin (R), Pyrazinamide (Z), Ethambutol (E)]](https://image.slidesharecdn.com/tb-230504152632-6986cab4/85/TB-pptx-30-320.jpg)





